Session Information
Date: Wednesday, October 24, 2018
Title: 6W006 ACR Abstract: Imaging of Rheumatic Diseases II: Ultrasound (2904–2909)
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose:
Musculoskeletal ultrasound is increasingly being used as a tool to assess inflammatory burden in rheumatoid arthritis (RA). Ultrasound-based outcome measures include power Doppler (PD) and grey scale synovial hypertrophy and have been assessed on fixed sets of between 5 to 78 joints. Although scanning large numbers of joints may be feasible in clinical trials, it may not be practical in clinical practice. We therefore evaluated a novel patient-specific method for constructing a longitudinal ultrasound outcome measure in RA patients.
Methods:
This was a 24 week, phase IV double blind open label clinical trial of 54 patients at 2 clinical centers with RA by 1987 ACR criteria and moderate to severe disease, treated with IV tocilizumab at initial dose of 4mg/kg. Patients not achieving DAS28-ESR≤3.2 at 12 weeks dose escalated to 8mg/kg. Baseline patient characteristics plus labs, clinical exam of swollen and tender joints, and PD of 34 joints (bilateral MCP 1-5, PIP 1-5, midline and radioulnar wrist, knee, MTP 2-5) at baseline and at 4, 12, 16, and 24 weeks were collected.
Results:
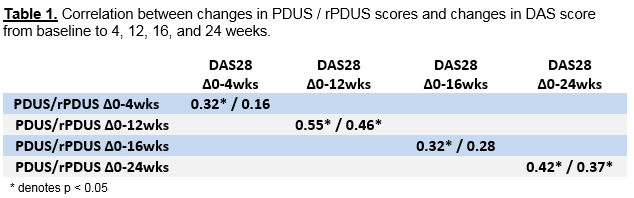
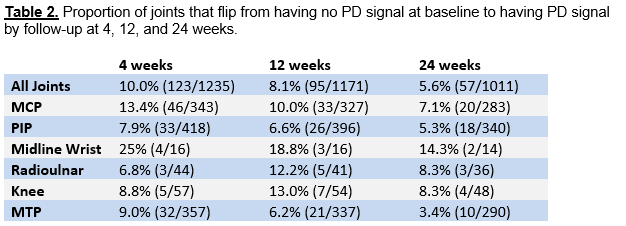
At each visit, PD score (PDUS) was computed as the sum of semi-quantitative PD signal for all joints (0-3 per joint, max 102). A novel patient-specific PD score was calculated from the reduced subset of joints with PD≥1 at baseline (rPDUS). Pearson correlation coefficients between 1) changes in PDUS and rPDUS versus changes in DAS, and 2) changes in PDUS versus changes in rPDUS were used to assess each outcome measure’s response to therapy from baseline to follow-up periods. The proportion of joints without PD signal at baseline that later developed PD signal (“flipped”) was estimated.
54 RA patients with mean age 51.9 ± 15.2 years, 91% female, 61.5% Caucasian, 85% seropositive, mean disease duration 10.0 ± 10 years, 72% on background DMARD at baseline were enrolled. At baseline, 1236 of 1829 joints scanned (67.5%) did not have PD signal. Changes in PDUS and changes in DAS were moderately correlated over intervals 0-4 weeks, 0-12 weeks, 0-16 weeks, and 0-24 weeks. Changes in rPDUS also correlated with changes in DAS, though slightly less so than with PDUS (Table 1). PDUS and rPDUS scores were highly correlated with r = 0.91 to 0.97. The overall proportion of “flipped” joints was 8.1% at 12 weeks and 5.6% at 24 weeks, with greatest variability seen in the midline wrist and MTP (Table 2).
Conclusion:
In RA patients starting a biologic, scanning only joints with baseline power Doppler synovitis can substantially reduce the number of joints needing to be scanned at follow-up visits. This gain in feasibility comes at a cost of a small reduction in correlation with validated disease activity measures.
To cite this abstract in AMA style:
Kuo D, Kaeley G, Ben-Artzi A, Brook J, Floegel-Shetty A, Elashoff D, Ranganath VK. Synovitis Focused Ultrasound in Rheumatoid Arthritis: A Joint Reduction Strategy [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/synovitis-focused-ultrasound-in-rheumatoid-arthritis-a-joint-reduction-strategy/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/synovitis-focused-ultrasound-in-rheumatoid-arthritis-a-joint-reduction-strategy/