Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Weight loss in obese patients can reduce knee osteoarthritis (OA) pain, even when physical therapy and intra-articular injections have failed. The impacts of either non-surgical or surgical weight loss on knee OA pain have been reported separately, but few studies have assessed them conjointly. While the decrease in mechanical load helps, the contribution of metabolic changes is less clear. We aimed to compare biomarker changes with weight loss as predictors of knee pain improvement, and consider a threshold of total weight loss necessary for these changes.
Methods: Patients from the NYU Langone Weight Management program were screened for knee pain prior to bariatric surgery or the start of a medical weight loss (MWL) regimen. We excluded patients with autoimmune disease, recent malignancy, recent intra-articular knee injections, and lack of OA by Kellgren-Lawrence (KL) x-ray grading. The BMI, Knee Injury and Osteoarthritis Outcome Score (KOOS) for pain, and blood samples were obtained at baseline and 1, 3, 6 and 12 months for evaluation of pain and biomarker levels.
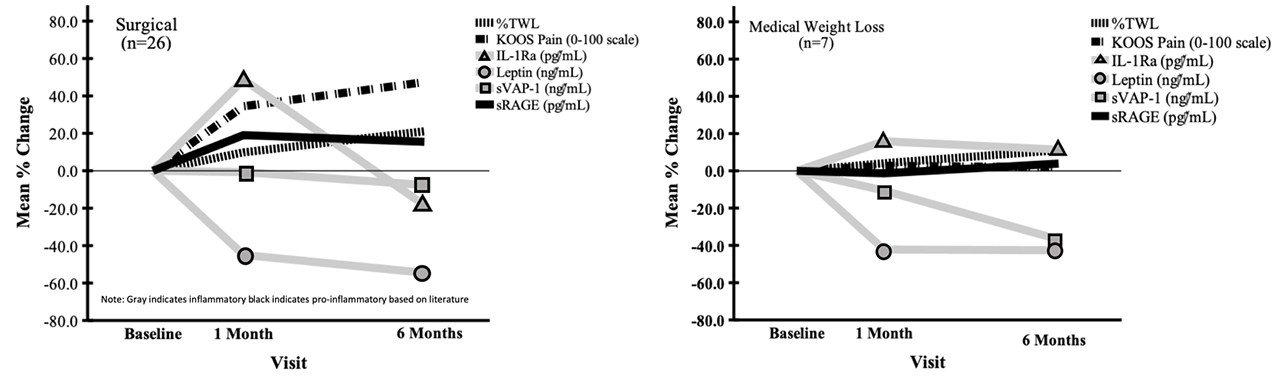
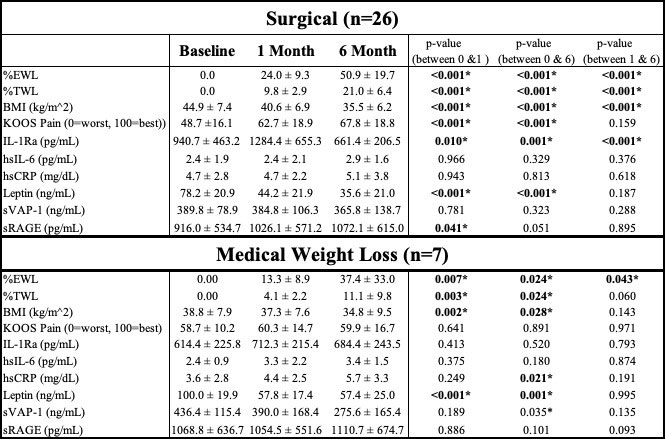
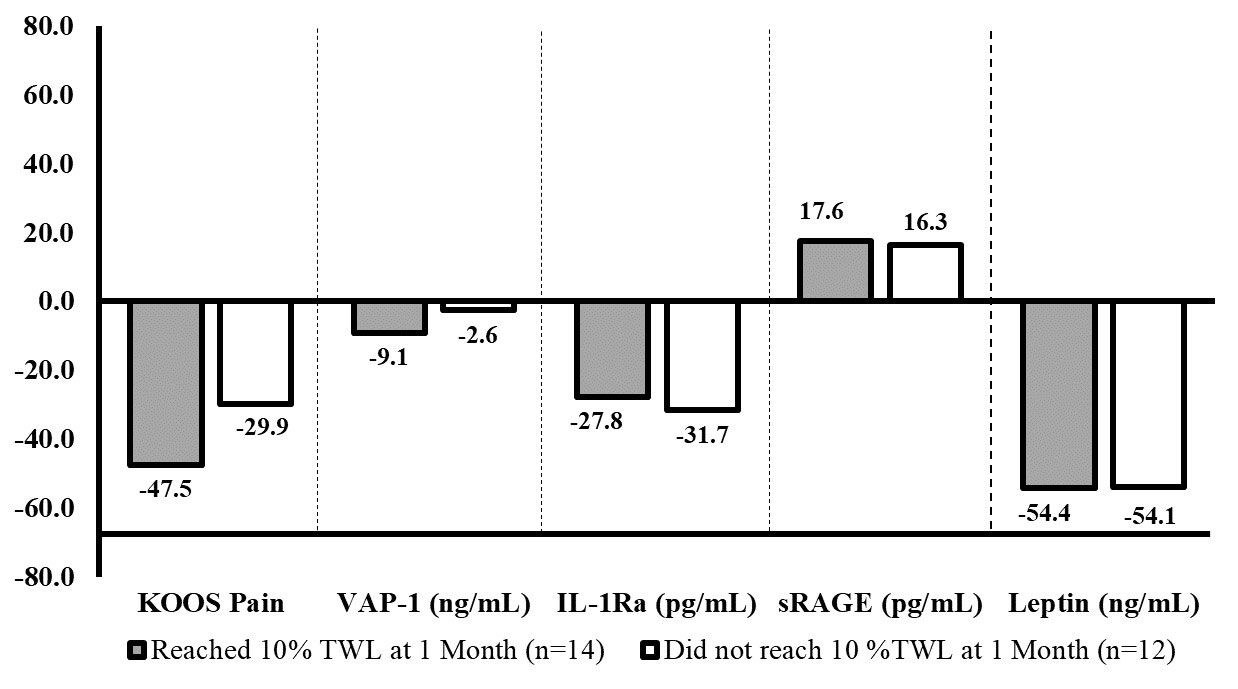
Results: Of 140 patients screened, 81 were eligible and enrolled (82.7% female; BMI 45.2±9.6 kg/m2, 31-74; age 52±12 years, 30-80). A total of 49 patients had surgery (10 bypass, 30 sleeve, 9 LapBand) and 24 medical weight loss. 33 patients completed visits up to 6 months (2 bypass, 18 sleeve, 6 LapBand, 7 MWL). By 1 month, the surgical patients had lost much more total weight than the MWL group (9.8% vs 4.1 %, p=0.001), and realized marked pain relief (p< 0.001). By 6 months both groups had continued to lose weight, proportionately greater for surgical patients with further pain improvement. (Figure 1) Leptin levels dropped at 1 and then 6 months with both methods of weight loss. The pro-inflammatory protein IL-1Ra decreased significantly by 6 months in the bariatric patients, but increased with the medical regimen across both time points. Soluble vascular adhesion protein 1 (sVAP-1), another pro-inflammatory protein that facilitates leukocyte infiltration, decreased at both the 1 and 6 month intervals – but much more in MWL than in surgical patients. Consistent with the literature, the anti-inflammatory soluble receptor for advanced glycation endproducts (sRAGE) mirrored KOOS pain improvement only in surgical patients and stabilized after 1 month, but did not change in the MWL group. (Table 1) In a subgroup analysis, the 14 surgical patients who lost at least 10% of total weight by 1 month had significantly less pain at 6 months than the 12 who did not meet the threshold (ΔKOOS 47.5 vs 29.9) but the biomarker levels were similar. (Figure 2)
Conclusion: Surgical and medically supervised weight loss both lead to significant decreases in adiposity, but only those having bariatric surgery realize significant pain relief. The anatomical changes of surgical (vs. medical) weight loss result in different metabolic cascades given divergent biomarker trends. Bariatric patients who lose more than 10 percent of total body weight within the first month are more likely to have better pain relief by 6 months, but the biomarker changes reflect anatomic intervention – and are not dependent on the degree of surgical weight loss.
To cite this abstract in AMA style:
Bomfim F, Chen S, Zak S, Jazrawi T, Kundler M, Qie V, Peralta L, Aleman J, Ren-Fielding C, Lofton H, Patel J, Attur M, Abramson S, Samuels J. Surgical and Medical Weight Loss Threshold Dictates Decreases in Knee Osteoarthritis Pain but Not Reductions in Inflammatory Biomarkers [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/surgical-and-medical-weight-loss-threshold-dictates-decreases-in-knee-osteoarthritis-pain-but-not-reductions-in-inflammatory-biomarkers/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/surgical-and-medical-weight-loss-threshold-dictates-decreases-in-knee-osteoarthritis-pain-but-not-reductions-in-inflammatory-biomarkers/