Session Information
Date: Sunday, November 13, 2022
Title: Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Exposure to sunlight has been implicated as a major contributing factor in the pathogenesis of systemic lupus erythematosus (SLE) and juvenile dermatomyositis (JDM). Despite this evidence, assuring adequate sunscreen use in the pediatric rheumatology population remains a challenge and investigations into barriers to usage are inadequate. Similarly, the American Academy of Pediatrics recommends routine sun protective counseling, yet studies have shown suboptimal sunscreen use in the general pediatric population (13-34%). This study aims to investigate sun protection practices in patients of a pediatric rheumatology clinic.
Methods: We developed a survey that was offered to patients at routine visits in the pediatric rheumatology clinic at the Children’s Hospital at Montefiore, Bronx, NY. Patients surveyed had a variety of photosensitive and non-photosensitive conditions, including SLE, JDM, cutaneous lupus erythematosus (CLE), Juvenile Idiopathic Arthritis, and scleroderma. The survey was collected electronically via the Einstein-Montefiore REDCap (Research Electronic Data Capture), a secure web-based application for data collection.
To examine the association between disease activity of photosensitive skin conditions and adequate sun protection, we used validated disease activity tools, including SLE Disease Activity Index (SLEDAI) for SLE patients, defining active disease as SLEDAI >4 and Childhood Myositis Assessment Scale (CMAS) for JDM patients, defining active disease as CMAS< 45. Patient and physician global assessment (a 10cm VAS) were used as well, defining active disease >2 for each. Adequate sunscreen use was defined as reported sunscreen use daily or most days. Chi-square test was used to compare the different groups.
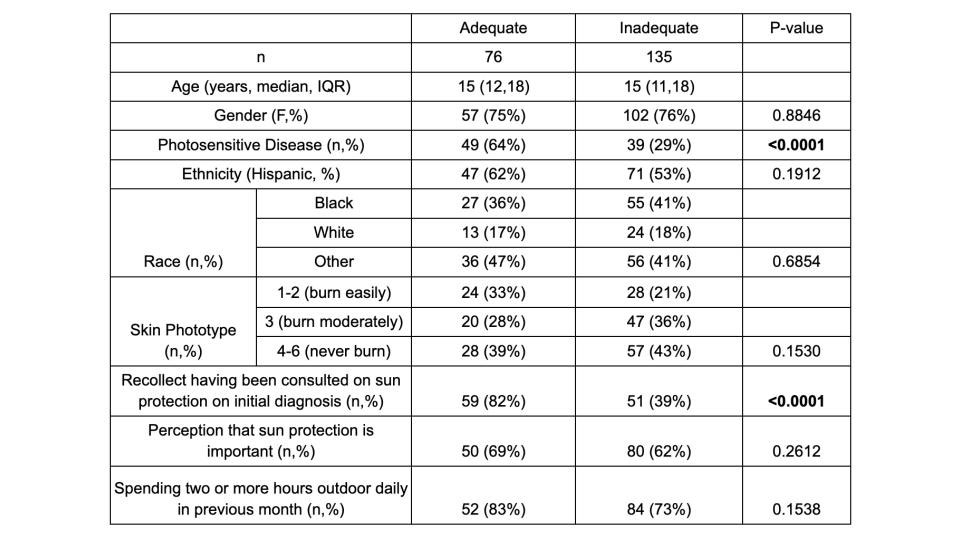
Results: We have enrolled 211 patients. Of these, 88 (42%) were diagnosed with a photosensitive skin condition including SLE, JDM or CLE. The median age was 15 years old (IQR 12, 18) with 75% female gender. Race and ethnicity were self-reported with 56% of patients identifying as Hispanic ethnicity; for race, 39% identified as Black, 18% white, 43% other. Most patients identified as having darker skin by the Fitzpatrick scale. While 62% of patients agreed that sun protection is important, only 36% overall reported appropriate sunscreen use. Factors associated with adequate sunscreen use were having a photosensitive skin condition (P< 0.0001) and recall of counseling on sunscreen use at initial diagnosis (P< 0.0001) (Table 1). When examining the association between disease activity and adequate sunscreen use, no statistically significant association was found. Seasonal variation of adequate sun protection was observed in patients with photosensitive conditions (figure 1). Less than 50% reported adequate sunscreen use in the winter as opposed to other seasons.
Conclusion: This study identifies gaps in sun protection use in a large proportion of pediatric patients with rheumatologic diseases, including those with photosensitive skin diseases. Patient counseling and education may be a key factor for adequate sun protection, especially early on during the initial diagnosis.
To cite this abstract in AMA style:
Dubov T, Wahezi D, Rothschild E, Rubinstein T, Tanner T. Sun Protection Use in Patients Followed in a Pediatric Rheumatology Clinic in an Urban Setting [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/sun-protection-use-in-patients-followed-in-a-pediatric-rheumatology-clinic-in-an-urban-setting-2/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sun-protection-use-in-patients-followed-in-a-pediatric-rheumatology-clinic-in-an-urban-setting-2/