Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes I: Pre-Onset & Early RA (0479–0483)
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: According to guidelines, clinical arthritis is mandatory for diagnosing rheumatoid arthritis (RA). However, in the absence of clinical synovitis, imaging-detected subclinical synovitis is increasingly used instead, and considered as starting point for DMARD-therapy. We searched for evidence of the natural course and determined in arthralgia-patients with subclinical synovitis from three longitudinal cohorts the frequencies of non-progression to clinically apparent inflammatory arthritis (IA) (i.e ‘false-positives’).
Methods: Subclinical synovitis in hands or feet of arthralgia-patients was visualized with ultrasound (two cohorts, subclinical synovitis definition: greyscale≥2 and/or power doppler≥1) or MRI (one cohort, subclinical synovitis: synovitis score ≥1 by two readers). Patients were followed for 1-year on IA-development; two cohorts also had 3-year data. Analyses were stratified for anti-citrullinated protein antibody (ACPA).
Results: Subclinical synovitis at presentation was present in 36%, 41% and 31% in the three cohorts. Of the ACPA-positive arthralgia-patients with subclinical synovitis 54%, 44% and 68%, respectively, did not develop IA (Figure 1A). These percentages were even higher in the ACPA-negative arthralgia-patients: 66%, 85% and 89% (Figure 1A). Similar results were seen after 3-years follow-up (Figure 1B).
Conclusion: Replacing clinical arthritis by subclinical synovitis to identify RA introduces a high false positive rate (44-89%). DMARD-initiation in absence of clinical arthritis may lead to considerable overtreatment.
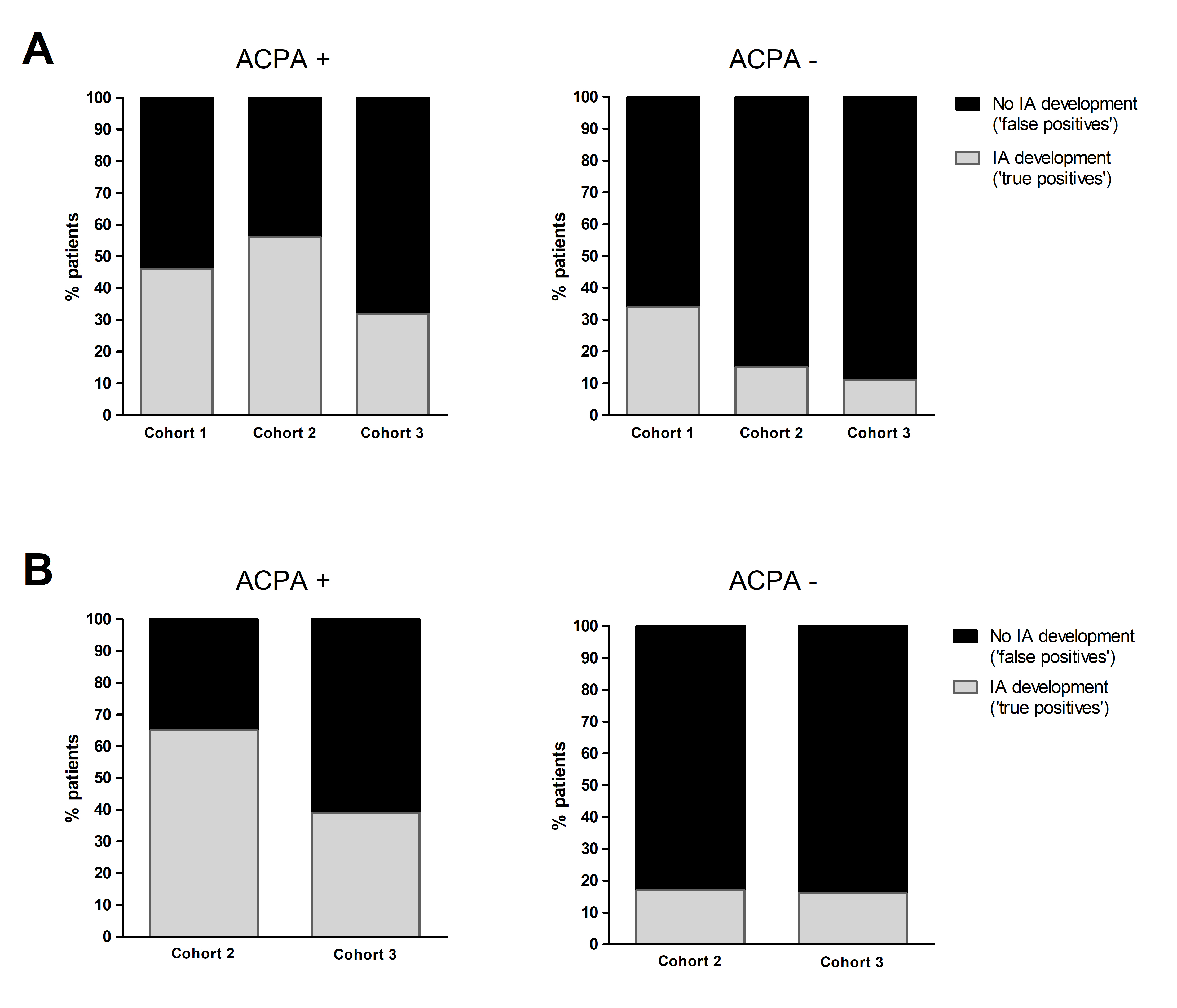 Figure 1 Percentage of arthralgia-patients with subclinical synovitis at baseline that did and did not develop inflammatory arthritis after 1-year (A) and 3-years follow-up (B), stratified for ACPA-status. Legend: (A) Percentage of patients with subclinical synovitis at baseline that did and did not progress to inflammatory arthritis after one year follow-up in three independent cohorts (ACPA-positive patients n=13, n=36, n=31, respectively; ACPA-negative patients n=47, n=157, n=19, respectively). (B) Percentage of patients with subclinical synovitis at baseline that did and did not progress to inflammatory arthritis after three year follow-up, in two independent cohorts (ACPA-positive patients n= 26, n=31, respectively; ACPA-negative patients n=121, n=19, respectively).
Figure 1 Percentage of arthralgia-patients with subclinical synovitis at baseline that did and did not develop inflammatory arthritis after 1-year (A) and 3-years follow-up (B), stratified for ACPA-status. Legend: (A) Percentage of patients with subclinical synovitis at baseline that did and did not progress to inflammatory arthritis after one year follow-up in three independent cohorts (ACPA-positive patients n=13, n=36, n=31, respectively; ACPA-negative patients n=47, n=157, n=19, respectively). (B) Percentage of patients with subclinical synovitis at baseline that did and did not progress to inflammatory arthritis after three year follow-up, in two independent cohorts (ACPA-positive patients n= 26, n=31, respectively; ACPA-negative patients n=121, n=19, respectively).
To cite this abstract in AMA style:
Rogier C, Wouters F, van Boheemen L, van Schaardenburg D, de Jong P, van der Helm - van Mil A. Subclinical Synovitis in Arthralgia: How Often Does It Result in Clinical Arthritis? A Longitudinal Study to Reflect on Starting Points for DMARD Treatment [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/subclinical-synovitis-in-arthralgia-how-often-does-it-result-in-clinical-arthritis-a-longitudinal-study-to-reflect-on-starting-points-for-dmard-treatment/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subclinical-synovitis-in-arthralgia-how-often-does-it-result-in-clinical-arthritis-a-longitudinal-study-to-reflect-on-starting-points-for-dmard-treatment/
