Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Assessment of disease activity in psoriatic arthritis (PsA) is based on tender and swollen joint counts (TJC and SJC, respectively). Yet, the prevalence of subclinical synovitis in patients in clinical remission is unknown. The purpose of this study is to estimate the MRI-detected prevalence and distribution of subclinical inflammatory changes of hands joints in patients with PsA in remission based on physical examination in comparison to active disease and to determine the sensitivity and specificity of physical examination findings using MRI-verified pathology as the standard of reference.
Methods: One-hundred consecutive, prospectively recruited patients with peripheral PsA (CASPAR criteria) underwent clinical evaluation and MRI of a predominantly involved hand performed within 72 hours from the clinical examination. Metacarpophalangeal (MCP), proximal (PIP) and distal interphalangeal (DIP) joints were scored according to the OMERACT PsAMRIS performed by an expert musculoskeletal radiologist, blinded for clinical data.
Results: Clinical characteristics and prevalence of MRI findings of the whole study cohort (n=100) and subgroups stratified by normal (TJC and/or SJC=0) (n=43) and abnormal clinical examination (n=57) are presented in Tables 1 and 2, respectively. Patients with active disease were older, had higher BMI, and longer duration of PsA compared to patients in clinical remission, 53.6±11.8 vs 48±13.0 years, p=0.025; 28.6±4.9 vs 26.3±4.9, p=0.021; 11.6 ±12.9 vs 8.1 ± 8.1 years, p=0.085, respectively. Otherwise, both subgroups were comparable in severity of psoriasis and treatment modalities. Total PsAMRIS and PsAMRIS of PIP joints were significantly higher in patients with active disease compared to patients in clinical remission, 9.8±18.4 vs 2.74±4.7, p=0.016 and 3.1±7.2 vs 0.6±1.4, p=0.026, respectively, with the same, though non-significant, trend for PsAMRIS of MCP and DIP joints. The overall prevalence of MRI inflammatory lesions in patients in clinical remission was low. Yet, subclinical synovitis was detected in 37.2% of patients, predominantly distributed in the MCP joints (37.2%), followed by equally affected PIP and DIP joints (11.6%). Flexor tenosynovitis and bone marrow edema were equally present in 11.6%, and periarticular inflammation in 2.3 %. The prevalence of MCP synovitis and flexor tenosynovitis was higher in patients with active disease but did not reach a statistical significance, whereas the difference was significant for other inflammatory MRI parameters (Table 2).
The sensitivity and specificity of physical examination of hand (TJC and/or SJC ≥1) for the corresponding MRI-detected synovitis were 66% and 51%, respectively, and for a combined MRI global inflammation score, including a summation of all the PsAMRIS components, were 69% and 63%, respectively.
Conclusion: MRI-detected subclinical synovitis, represented mainly as synovitis of MCP joints and flexor tenosynovitis was detected in up to third of PsA patients with a normal clinical hand examination. Further research is required to assess the pathogenetic role of subclinical hand inflammation for structural progression.
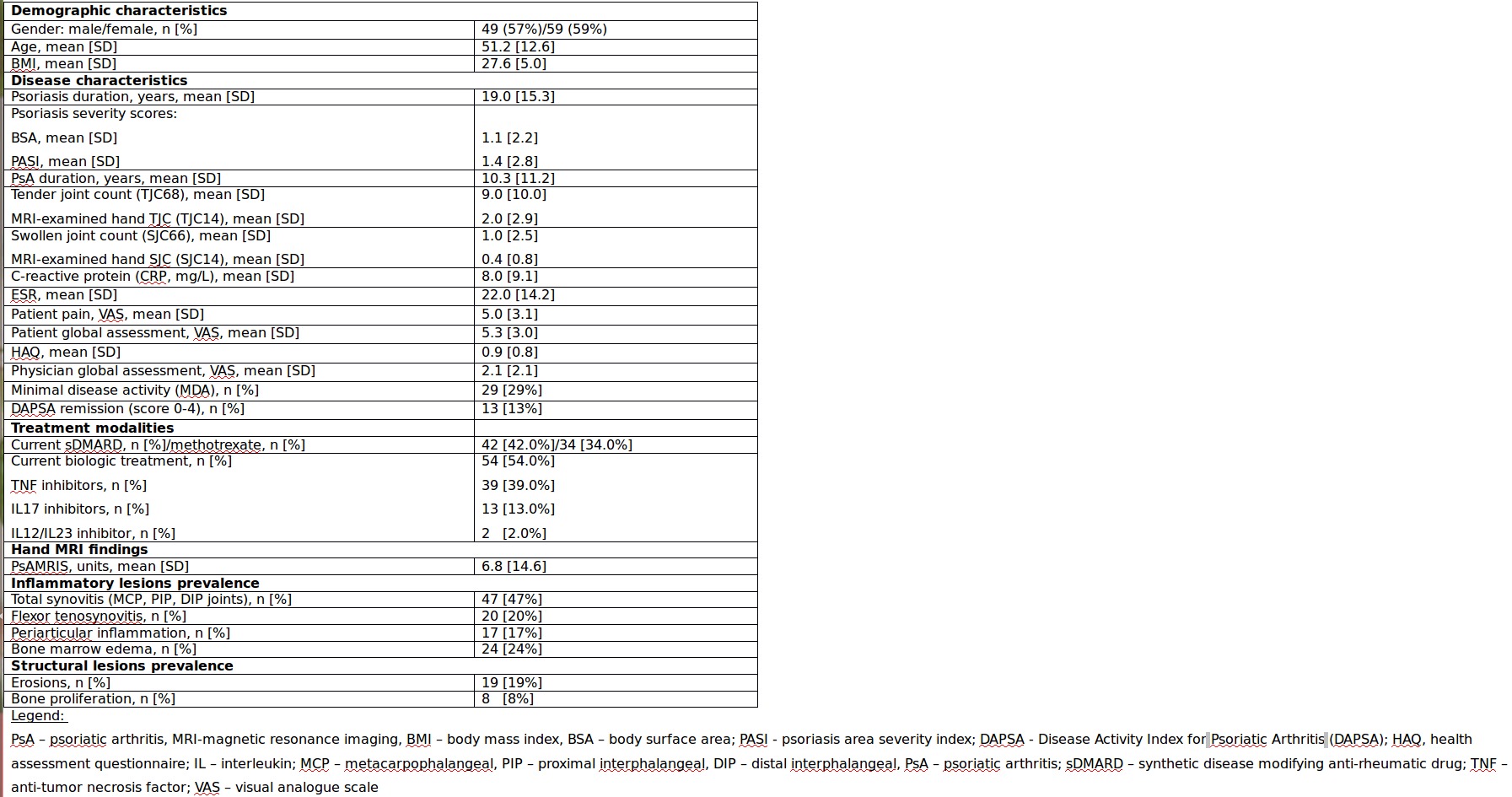 Table 1. Clinical characteristics and hand MRI findings in the PsA cohort.
Table 1. Clinical characteristics and hand MRI findings in the PsA cohort.
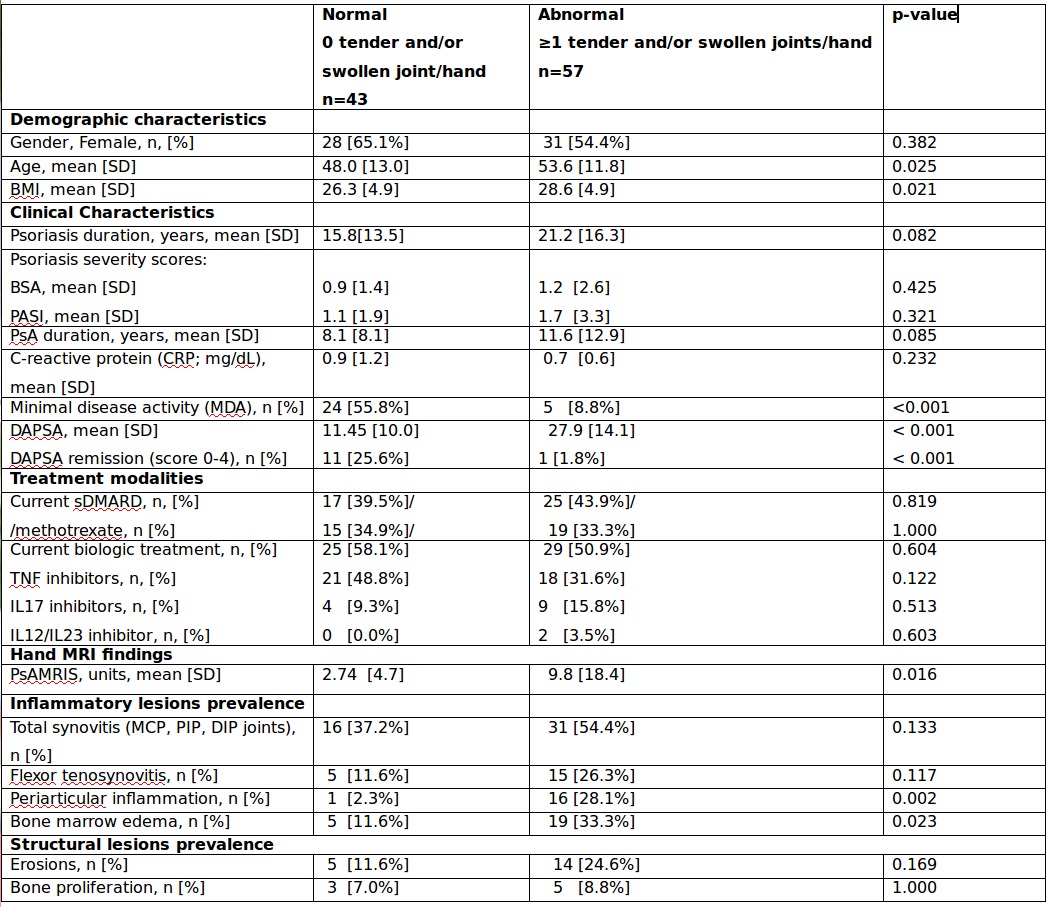 Table 2. Clinical characteristics in PsA patients and hand MRI findings stratified by normal versus abnormal clinical examination of hand joints.
Table 2. Clinical characteristics in PsA patients and hand MRI findings stratified by normal versus abnormal clinical examination of hand joints.
To cite this abstract in AMA style:
Furer V, Polachek A, Levartovsky D, Wollman J, Zureik M, Paran D, Sarbagil-Maman H, Borok Lev-Ran S, Berman M, Kaufman I, Broide A, Aloush V, Lahat goldstein Y, Nevo S, Eshed I, Elkayam O. Subclinical Joint Inflammation of Hands by Magnetic Resonance Imaging in Patients with Psoriatic Arthritis in Clinical Remission Compared to Active Disease [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/subclinical-joint-inflammation-of-hands-by-magnetic-resonance-imaging-in-patients-with-psoriatic-arthritis-in-clinical-remission-compared-to-active-disease/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subclinical-joint-inflammation-of-hands-by-magnetic-resonance-imaging-in-patients-with-psoriatic-arthritis-in-clinical-remission-compared-to-active-disease/
