Session Information
Date: Sunday, November 17, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Subclinical GCA in PMR has been estimated to affect 1 in 5 patients as assessed by vascular ultrasound [1, 2]. This study compared the ultrasound phenotype of subclinical GCA in PMR with patients with GCA patients and assessed whether baseline quantitation with halo count (HC), halo score (HS), or OMERACT GCA Ultrasonography Score (OGUS) in subclinical GCA in PMR predicted relapse during the first 12 months of treatment.
Methods: HS, HC, and OGUS scores were calculated on patients with ultrasound-identified subclinical GCA in PMR (sGCA/PMR) from a multi-centre European prospective cohort study and compared with a prospective Irish GCA cohort. All patients had a similar corticosteroid tapering in keeping with the ACR/ EULAR PMR and GCA guidelines [3, 4]. Statistical analysis was completed with the paired t-test and Pearson’s correlation coefficient.
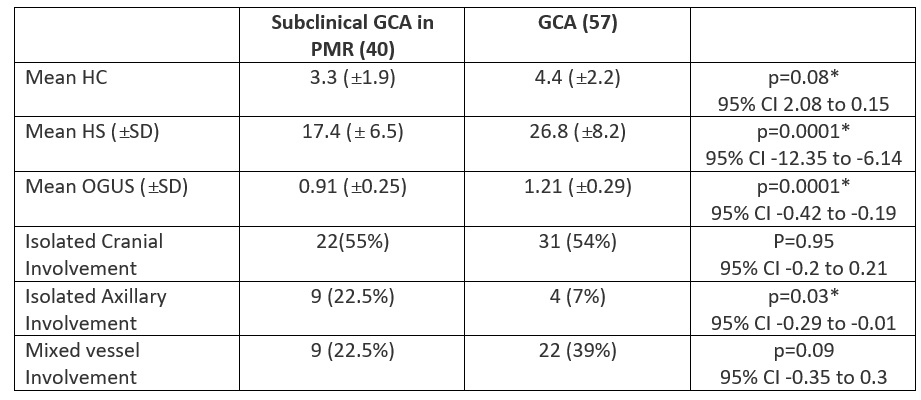
Results: 40 patients with sGCA/PMR were compared with 57 patients with GCA. 22.5% of sGCA/PMR had isolated axillary involvement compared with only 7% in GCA, p=0.03 (95% CI -0.29 to -0.01). Similar numbers in both groups had isolated cranial vessel involvement and mixed vessel involvement. The number of involved vessels as assessed by the mean HC in both sGCA/PMR and GCA patients was not significantly different at 3.3 and 4.4 respectively, p=0.08 (95% CI 2.08 to 0.15). However, the severity of vascular inflammation was significantly different with a mean HS of 17.4 in sGCA/PMR compared with 26.8 in GCA, p=0.0001 (95% CI -12.35 to -6.14). The mean OGUS between the two groups was also significantly different at 0.91 in sGCA/PMR and 1.21 in GCA, p=0.0001 (95% CI -0.42 to -0.19). One patient was excluded from the relapse analysis due to being on tocilizumab treatment. While there was a positive correlation between OGUS scores in sGCA/PMR and risk of relapse, this was not statistically significant r=0.15; p=0.36. Baseline OGUS scores in the GCA cohort correlated well with relapse in the first 12 months with r=0.31, p< 0.0005.
Conclusion: Subclinical GCA in PMR has a different ultrasonographic phenotype to GCA. While the number of involved arteries in both disease groups was similar, the pattern of involvement was different with those with sGCA/PMR having significantly more isolated axillary artery involvement. The severity of vascular inflammation as quantified by HS and OGUS was significantly higher in GCA which may explain why the arterial involvement in sGCA/PMR was asymptomatic. A higher OGUS score at baseline predicted relapse for GCA patients but not for patients with subclinical GCA in PMR.
To cite this abstract in AMA style:
Cowley S, Harkins P, Kirby C, Conway R, Kane D, Karalilova R, Macchioni P, Ponte C, Conticini E, Tomelleri A, Monti S, monjo i, Batalov Z, Klinowski G, Falsetti P, Campochiaro C, Hocevar A, De Miguel E. Subclinical Giant Cell Arteritis in Polymyalgia Rheumatica Has a Different Vascular Ultrasound Phenotype Than Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/subclinical-giant-cell-arteritis-in-polymyalgia-rheumatica-has-a-different-vascular-ultrasound-phenotype-than-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subclinical-giant-cell-arteritis-in-polymyalgia-rheumatica-has-a-different-vascular-ultrasound-phenotype-than-giant-cell-arteritis/