Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The amygdala, a limbic structure of the brain’s salience network, links chronic external stressors with downstream effects on the HPA axis and hematopoietic tissues that modulate cortisol production, activate immune effector cells, and induce inflammatory cytokine production. Higher resting metabolic amygdala activity relative to cortical activity (AmygAc) has been linked to systemic and arterial inflammation and cardiovascular disease (CVD) in the general population. However, whether AmygAc plays a role in RA, a disease characterized by inflammation and a heightened risk of CVD, has never been explored.
Methods: In a clinical trial of the effect of immunomodulators on arterial inflammation, people with active RA despite MTX were randomly assigned to the addition of either a TNF inhibitor (TNFi) or triple therapy. Baseline whole body 18F-flourodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) scans were assessed for the maximal and mean uptake of FDG in the bilateral amygdala and bilateral temporal lobes. AmygAc was assessed as amygdalar activity relative to temporal lobe activity. The change in arterial inflammation over 24 weeks was measured as the maximal arterial target-to-blood background ratio (TBR) of FDG uptake in the most diseased segment (MDS) of either the carotid arteries or aorta (TBRmax MDS). The associations of AmygAc with RA characteristics and arterial inflammation were assessed using generalized linear models adjusting for relevant confounders.
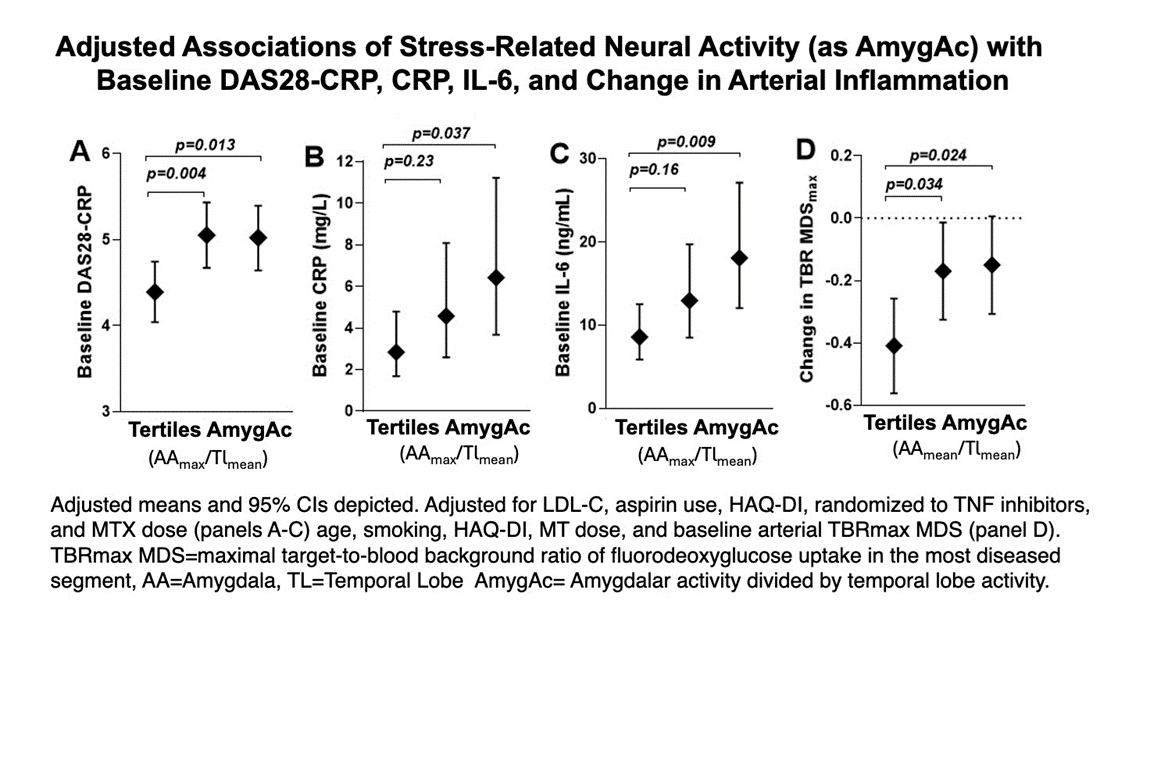
Results: A total of 91 RA patients [mean age=60 years; 71% female; median RA duration=1.8 years; 57%; median baseline DAS28-CRP=4.9] had interpretable AmygAc. AmygAc was significantly associated with baseline DAS28-CRP (Figure panel A), such that the mean adjusted DAS28-CRP was 0.73 units (17%) higher for those in the 2nd or 3rd tertiles of AmygAc compared with the 1st tertile (p=0.002 comparing the 1st vs the combined 2nd and 3rd tertiles). The same relationships were observed for all domains of the DAS28 except not significantly for the swollen joint count. There was a linear association of AmygAc with both CRP and IL-6 (Figure panels B & C). These associations were similar in subgroups defined by age, sex, BMI, CVD risk factors, seropositivity, randomized treatment, NSAID use, and reported stress and depressive symptoms. Those with higher baseline AmygAc were not resistant to treatment with either TNFi or triple therapy, as the final DAS28-CRP did not differ according to baseline AmygAc. While AmygAc was not significantly associated with the baseline arterial TBRmax MDS, it was significantly associated with the change in TBRmax MDS (figure panel D), such that the improvement in arterial inflammation for those in the 1st tertile of AmygAc was more than double that of the 2nd and 3rd tertiles (p=0.011). The association of AmygAc with the change in arterial inflammation did not differ according to randomized treatment.
Conclusion: These findings highlight unstudied potential links between stress-related neural activity with disease activity, systemic inflammation, and effectiveness of immunomodulators on arterial inflammation in people with RA that may be targets for novel interventions.
To cite this abstract in AMA style:
Giles J, Bathon J, Liao K, Rist P, Abohashem S, Osborne M, Civieri G, Fayad Z, Solomon D, Tawakol A. Stress-Related Neural Activity Measured with FDG-PET/CT Is Associated with Articular Disease Activity, Systemic Inflammation, and Treatment-associated Change in Arterial Inflammation in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/stress-related-neural-activity-measured-with-fdg-pet-ct-is-associated-with-articular-disease-activity-systemic-inflammation-and-treatment-associated-change-in-arterial-inflammation-in-rheumatoid-art/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/stress-related-neural-activity-measured-with-fdg-pet-ct-is-associated-with-articular-disease-activity-systemic-inflammation-and-treatment-associated-change-in-arterial-inflammation-in-rheumatoid-art/