Session Information
Date: Saturday, November 12, 2022
Title: SLE – Treatment Poster I
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Glucocorticoids are frequently employed in the treatment of systemic lupus erythematosus (SLE) patients and play a critical role in the induction therapy of lupus nephritis (LN), despite their many side effects, which include steroid-induced diabetes (SID). Information regarding SID in SLE patients is quite scant. The aim of this study is to determine risk factors associated with the development of SID in patients receiving induction therapy for LN.
Methods: A nested case-control study was conducted at a tertiary referral hospital in Mexico City. The analysis included patients with LN diagnosed with a renal biopsy between 2012 and 2017, who had received induction treatment which included steroids, and had a follow-up of at least one year after induction onset. Patients with a previous diagnosis of DM were excluded. Differences between the group of new SID cases and the control group were analyzed. A logistic regression analysis was performed to determine the variables associated with the development of SID.
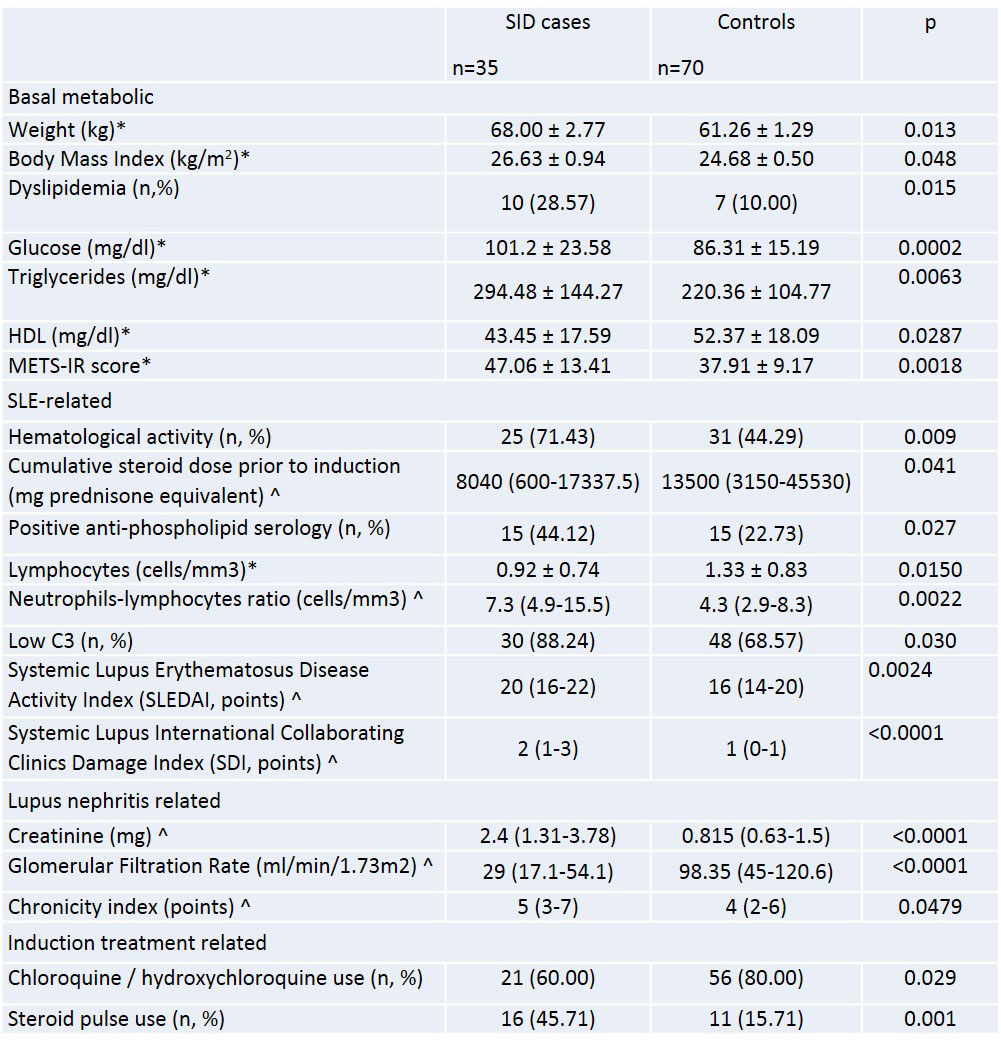
Results: We included 358 patients with LN, out of which 35 (9.77%) developed SID (cases). Two controls were selected for each case (n = 70). Regarding baseline characteristics at induction onset, the group of patients who developed SID had more metabolic risk factors when compared to the control group, as shown in Table 1. The metabolic score for insulin resistance (METS-IR) was also higher in patients with SID (p< 0.01). Concerning SLE-associated baseline variables, the SID group had a lower lymphocyte count (p=0.01), higher neutrophil/lymphocyte ratio (p< 0.01), in addition to higher SLEDAI (p< 0.01) and SLICC damage index (p< 0.01) scores. Interestingly, the cumulative pre-induction steroid dose was higher in controls (p=0.04). Lastly, regarding induction treatment, a higher percentage of patients who presented SID were given steroid pulses (p=0.001) and a lower percentage received antimalarials (p=0.02). The rest of the variables can be seen in Table 1.
After logistic regression, only the SLICC Damage Index score remained significantly associated with the development of SID (OR 3.64 95%CI 1.90-6.98, p< 0.0001), but there was a trend for SLEDAI (OR 1.13, 95%CI 0.99-1.28, p=0.06) and METS-IR (OR 1.06 95%CI 0.99-1.13, p=0.06) to be risk factors, and for treatment with antimalarial drugs to be protective (OR 0.32, 95%CI 0.08-1.2, p=0.09).
Finally, the proportion of patients who fulfilled the criteria for DM after three years of follow-up was analyzed, and it was found to be 11.4% of the cases and, interestingly, none in the controls (OR 20.1 95%CI 1.05–385, p=0.01).
Conclusion: SDI development in patients receiving induction therapy for LN is associated with both classic metabolic risk factors and SLE-specific factors. Antimalarial use during induction could be associated with a protective effect. Rheumatologists should be aware of this potential complication, in order to implement appropriate detection and treatment strategies.
To cite this abstract in AMA style:
Dimas Ramírez C, Fortanell-Meza A, San Agustin-Morales D, Brenner Muslera E, Mejia-Vilet J, Almeda-Valdes P, Vázquez Cárdenas P, Merayo-Chalico F, Barrera-Vargas A. Steroid-Induced Diabetes in Lupus Nephritis Patients: Classic Risk Factors or a Different Type of Diabetes? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/steroid-induced-diabetes-in-lupus-nephritis-patients-classic-risk-factors-or-a-different-type-of-diabetes/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/steroid-induced-diabetes-in-lupus-nephritis-patients-classic-risk-factors-or-a-different-type-of-diabetes/