Session Information
Date: Saturday, November 7, 2020
Title: Epidemiology & Public Health Poster II: OA, Osteoporosis, & Other Rheumatic Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Regular physical activity may have benefits for patients with rheumatoid arthritis (RA) and psoriatic arthritis (PsA), but patients with active disease are often reluctant to increase activity. Principles from behavioral economics (BE), a field combining psychology and economics, have been applied to motivate increased physical activity in non-arthritis patients. The objective of this study was to assess the feasibility and efficacy of a loss aversion financial incentive for increasing step counts and improving disease symptoms in RA and PsA patients with active disease.
Methods: A double-blind randomized controlled pilot trial was performed among patients with RA and PsA. Participants were required to have active disease defined by having at least one swollen joint and a Routine Assessment of Patient Index Data-3 (RAPID3) score >3 (range 0-30 with < 3 indicating remission). The primary goal of this study was to establish feasibility of the platform and study conduct. The primary outcome was change in RAPID3 between the two arms. The trial included two visits (Figure 1) and weekly check-ins via virtual trial platforms, Way to Health and the ArthritisPower app. Patients were given a Fitbit Alta at baseline and completed a two-week run-in period to assess average step count. Patients were then prompted to select a step count goal (30, 40, or 50% above baseline daily step count) and complete a commitment contract. After selection of a goal, participants randomized to the intervention arm received a financial loss aversion incentive (each month, patients started with $75 in their account and lost $2.50 for each day they did not reach their goal). All patients received weekly text message prompts providing feedback about their performance over the past week and completed weekly PROs. After 12 weeks of the intervention (at week 14), the incentive was removed and patients were followed to 26 weeks to determine how long the effect persisted.
Results: In the pilot trial, 71 patients were verbally consented for screening, 34 underwent screening (of these, two were ineligible), 27 were randomized, and 22 patients completed the 14-week study visit. The mean step count at baseline was 5,962. By 28 days, 65% of patients increased their step count. Participants receiving the incentive had an average of 714 more steps per day over the first 14 weeks and a greater probability of reaching 10,000 steps per day during follow-up (30% v. 21%, p=0.41). Among patients who achieved their step count goals more than 50% of days, we observed more improvement in sleep quality, fatigue, and overall well-being (p< 0.05) (Figure 2). After adjusting for baseline RAPID3, the 14-week RAPID3 scores were lower in the group that achieved their step goals 50% of the time [B: -3.91 (-11.8, 3.99); a difference that approximates the minimal clinically important difference (MCID) for the RAPID3 (3.6).
Conclusion: While financial incentives have worked well in patients without arthritis, the estimated effect of the financial incentive in this small study was more modest in patients with RA and PsA. Those that were able to increase their physical activity and meet their step goals had greater improvements in symptoms over the course of the study.
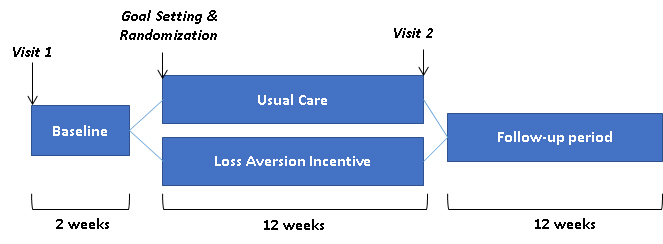 Figure 1. Study diagram. There were two study visits (weeks 0 and 14). The first two weeks served as a baseline period to establish a baseline step count. Patients then selected a step count goal which was either 30%, 40%, or 50% above the baseline step count and signed a commitment contract. Patients were then randomized to a financial incentive or no incentive. The primary outcome (change in RAPID3) occurred at week 14.
Figure 1. Study diagram. There were two study visits (weeks 0 and 14). The first two weeks served as a baseline period to establish a baseline step count. Patients then selected a step count goal which was either 30%, 40%, or 50% above the baseline step count and signed a commitment contract. Patients were then randomized to a financial incentive or no incentive. The primary outcome (change in RAPID3) occurred at week 14.
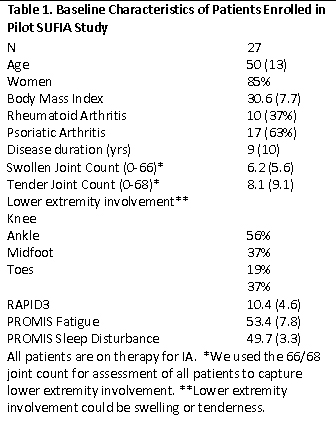 Table 1. Baseline Characteristics of Patients Enrolled in Pilot SUFIA Study
Table 1. Baseline Characteristics of Patients Enrolled in Pilot SUFIA Study
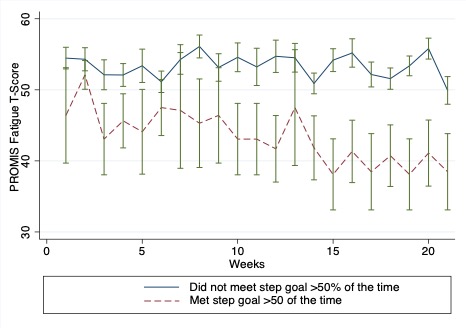 Figure 2: Change in fatigue severity among those with greater adherence to step count goals. The PROMIS fatigue score increases with worse fatigue and decreases with improving fatigue.
Figure 2: Change in fatigue severity among those with greater adherence to step count goals. The PROMIS fatigue score increases with worse fatigue and decreases with improving fatigue.
To cite this abstract in AMA style:
Ogdie A, Bush K, George M, Patel M, Nowell W, Gavigan K, Curtis J, Baker J. Stepping up for Inflammatory Arthritis (SUFIA): A Pilot Trial to Test Behavioral Economics Strategy to Increase Physical Activity in Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/stepping-up-for-inflammatory-arthritis-sufia-a-pilot-trial-to-test-behavioral-economics-strategy-to-increase-physical-activity-in-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/stepping-up-for-inflammatory-arthritis-sufia-a-pilot-trial-to-test-behavioral-economics-strategy-to-increase-physical-activity-in-inflammatory-arthritis/
