Session Information
Date: Sunday, November 12, 2023
Title: (0380–0422) RA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cholesterol efflux capacity (CEC) is the main antiatherogenic function of high-density lipoprotein (HDL). ATP-binding-cassette A1 (ABCA1) membrane transporter initiates cholesterol export from arterial macrophages to pre-β HDL particles fostering their maturation; in turn, those accept cholesterol through ABCG1-mediated export. Impaired pre-βHDL maturation may disrupt the collaborative function of the two transporters and adversely affect atherosclerosis. Statins exert atheroprotective functions systemically and locally on plaque. We here evaluated associations between ABCA1-CEC, coronary atherosclerosis and cardiovascular risk and the influence of statins on those relationships in rheumatoid arthritis (RA).
Methods: Atherosclerosis (noncalcified, partially or fully calcified, low attenuation plaques) was evaluated with coronary computed tomography angiography in 140 patients without cardiovascular disease and reassessed in 99 after 6.9±0.4 years. ABCA1-CEC and ABCG1-CEC were measured in J774 macrophages and Chinese hamster ovary cells respectively as previously described. Cox regression evaluated the association between ABCA1-CEC and cardiovascular risk. Multivariable negative binomial and robust logistic regression tested associations of ABCA1-CEC and its interactions with statin therapy on coronary plaque burden at baseline and its progression respectively.
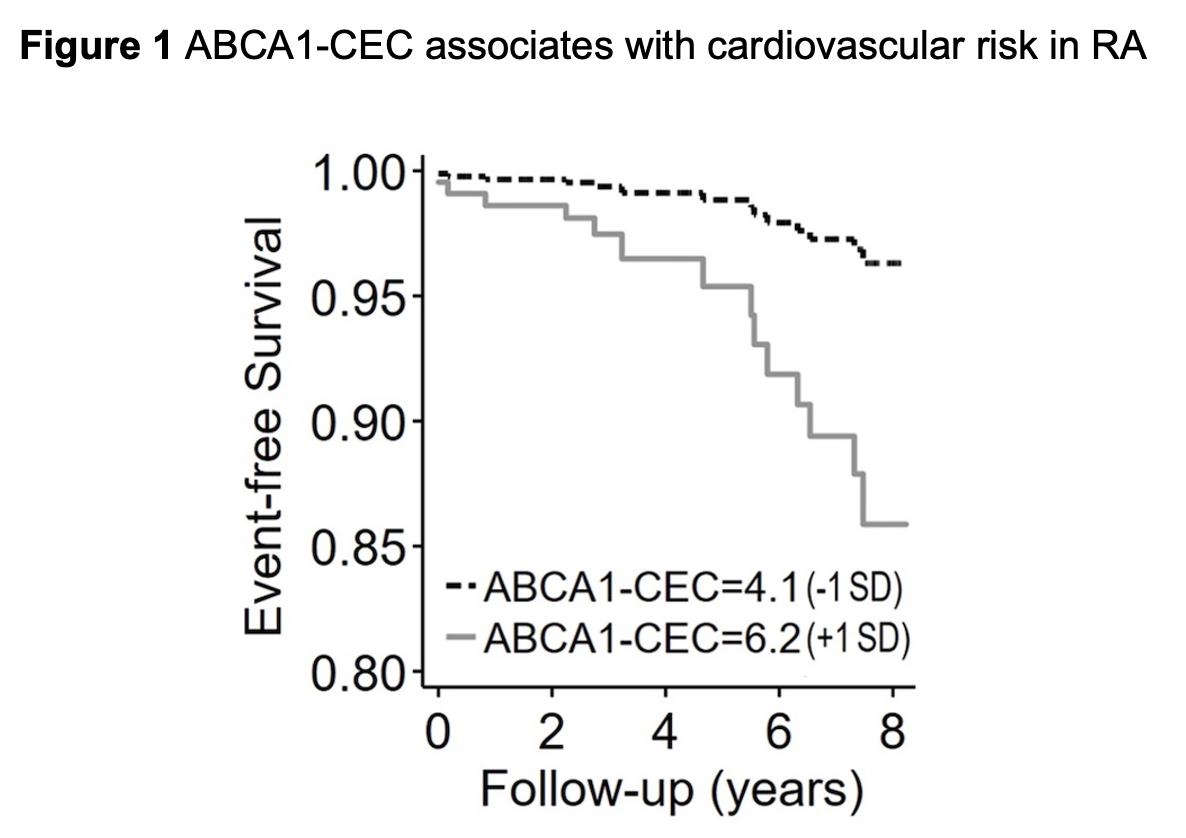
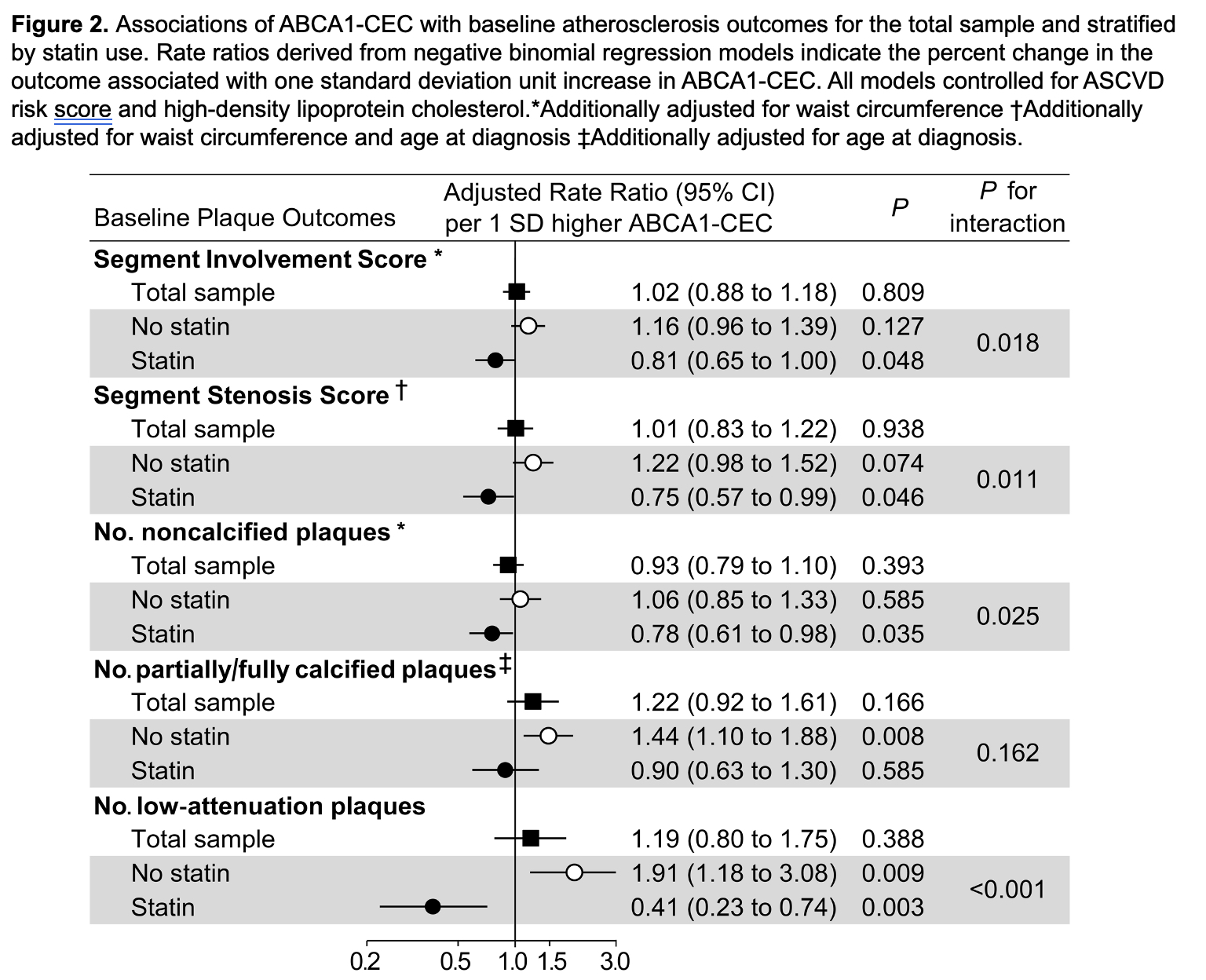
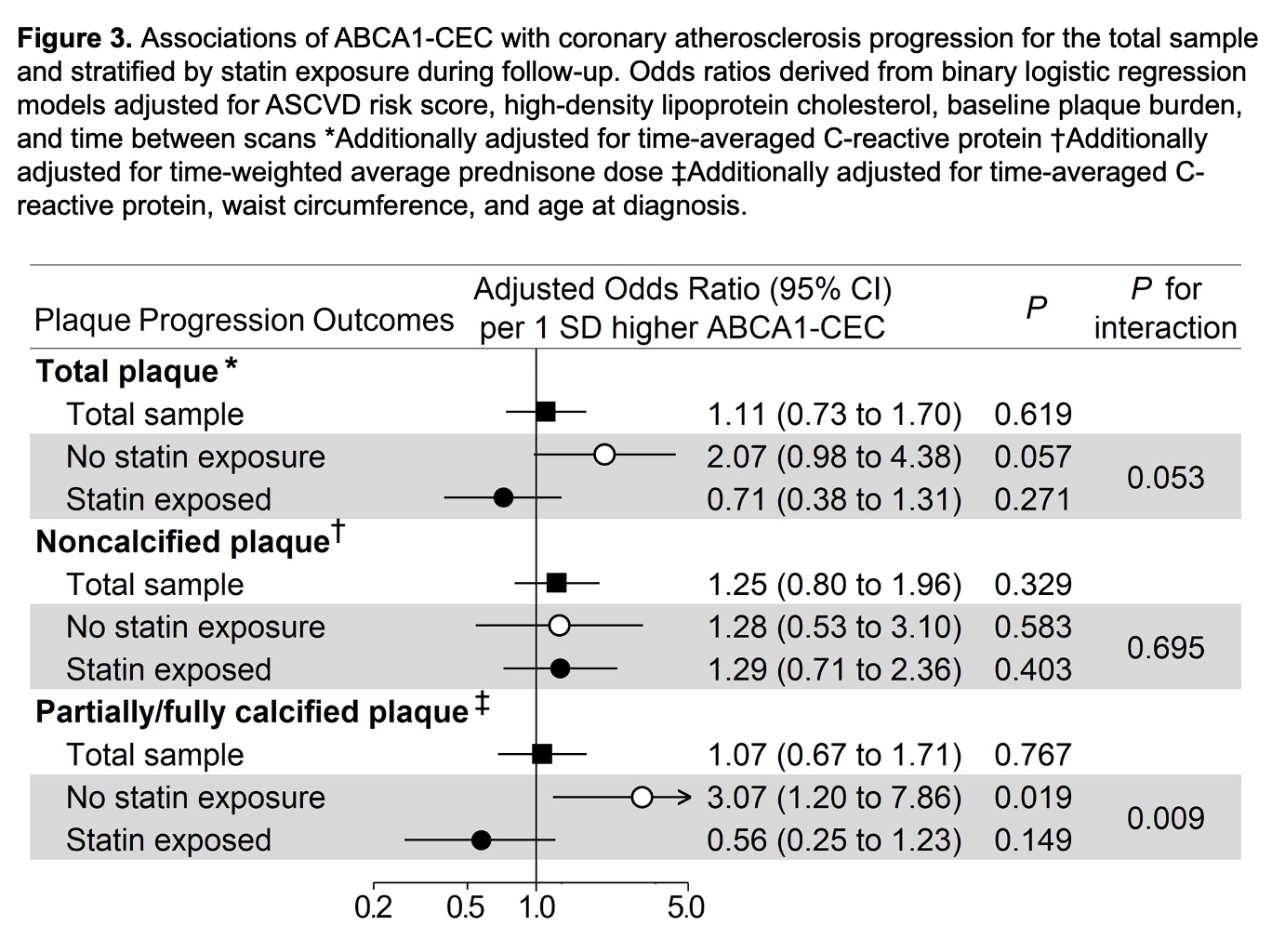
Results: ABCA1-CEC inversely correlated with ABCG1-CEC (Pearson r= -0.167, p=0.049). ABCA1-CEC (per SD increment) associated with long-term cardiovascular event risk after adjustments for cardiovascular risk score and baseline plaque burden [HR 2.05 (95% CI 1.20-3.48), Figure 1]. There was an interaction of ABCA1-CEC with time-varying statin use (p=0.038) such that current statin use inversely associated with risk only in patients with ABCA1-CEC below the upper tertile. ABCA1-CEC had no main effect on plaque or plaque progression; instead, ABCA1-CEC (per SD) associated with fewer baseline total plaques (adjusted rate ratio [aRR] 0.81, [95%CI 0.65-1.00]), noncalcified plaques (aRR 0.78 [95%CI 0.61-0.98]), and low attenuation plaques (aRR 0.41 [95%CI 0.23-0.74]) in statin users, and more low attenuation plaques (aRR 1.91 [95%CI 1.18-3.08]) in nonusers (p-for-interaction=0.018, 0.011, 0.025 and < 0.001 respectively, Figure 2). Moreover, ABCA1-CEC (per SD) associated with greater partially/fully-calcified plaque progression (adjusted odds ratio 3.07 [95%CI 1.20-7.86]) only in patients not exposed to statins during follow-up (p-for-interaction=0.009, Figure 3).
Conclusion: In the context of inflammation and impaired pre-β HDL maturation typical of RA, higher ABCA1-CEC may reflect a proatherogenic rather than atheroprotective state, associated with greater coronary atherosclerosis burden, vulnerability and cardiovascular risk. Statin use, by reducing cell cholesterol overload and restoring pre-β HDL maturation may unmask and promote the atheroprotective effect of ABCA1-CEC.
To cite this abstract in AMA style:
Karpouzas G, Papotti B, Ormseth S, Palumbo M, Hernandez E, Adorni M, Zimetti F, Budoff M, Ronda N. Statins Influence the Relationship Between ATP-binding Cassette Transporter A1 (ABCA1)-mediated Cholesterol Efflux and Coronary Atherosclerosis in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/statins-influence-the-relationship-between-atp-binding-cassette-transporter-a1-abca1-mediated-cholesterol-efflux-and-coronary-atherosclerosis-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/statins-influence-the-relationship-between-atp-binding-cassette-transporter-a1-abca1-mediated-cholesterol-efflux-and-coronary-atherosclerosis-in-rheumatoid-arthritis/