Session Information
Date: Monday, November 18, 2024
Title: RA – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) patients have an increased risk of cardiovascular disease (CVD) partly due to accelerated atherosclerosis from chronic inflammation. However, this increased risk is not fully captured by conventional risk calculators. Statins are known to reduce cardiovascular events and mortality in patients and are commonly used for primary and secondary prevention of CVD. Our goals are to 1) Evaluate whether RA patients are more likely to receive statin therapy compared to patients with osteoarthritis (OA), and 2) Examine the influence of various covariates on statin prescription rates.
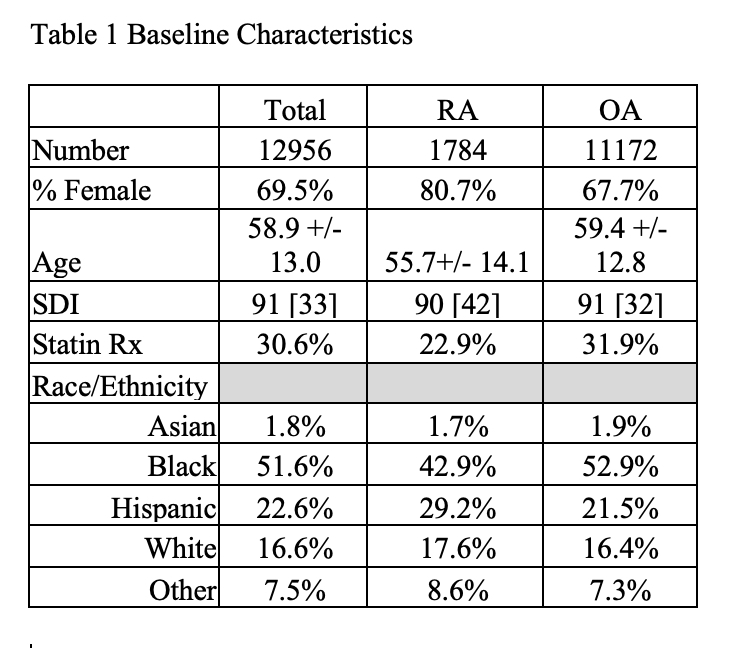
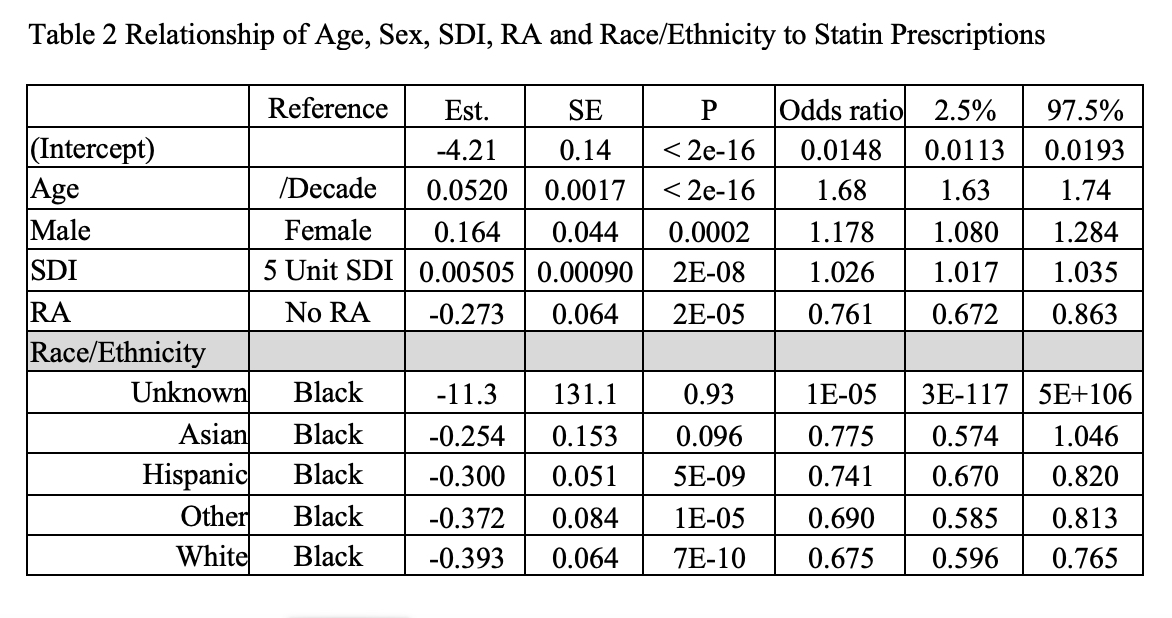
Methods: A retrospective cohort study was conducted at a large urban academic medical center using data collected between January 1, 2018, and September 12, 2020. Patients aged 18 or older and diagnosed with either RA or OA, but not both, were included in the study. RA and OA patients were identified based on ICD-10 diagnosis codes. OA patients were used as the comparison group because, unlike systemic rheumatologic diseases, OA is not considered a risk enhancer for CVD. Multivariate logistic regression was utilized to analyze the association between statin prescriptions and covariates, including age, sex, ethnicity, social deprivation index (SDI), and RA diagnosis.
Results: A total of 1784 RA patients and 11172 OA patients were included. We found that RA diagnosis was associated with a 24% lower likelihood of receiving statins (OR: 0.761, 95% CI: 0.672-0.863, p=2E-05). Logistic regression analysis indicated that age was significantly associated with statin prescriptions, with a 68% increase in likelihood for every decade of age (OR: 1.68, 95% CI: 1.63-1.74, p< 2e-16). Male sex was associated with an 18% increase in statin prescribing (OR: 1.178, 95% CI: 1.080-1.284, p=0.0002). SDI was positively associated with statin prescription (OR: 1.026 per 5-unit increase, 95% CI: 1.017-1.035, p=2e-08). Compared with Black patients, Asian, Hispanic, and White patients were less likely to receive statin prescriptions (Asian: OR: 0.775, 95% CI: 0.574-1.046, p=0.096; Hispanic: OR: 0.741, 95% CI: 0.670-0.820, p=5E-09; White: OR: 0.675, 95% CI: 0.596-0.765, p=7E-10).
Conclusion: Our study shows that RA patients were 24% less likely to receive statins compared with OA patients, despite their higher cardiovascular risk due to an underlying chronic inflammatory state. This suggests a potential underutilization of statins in RA patients, indicating the need for better awareness and management to reduce the high risk of CVD in the RA population. Furthermore, prescribing of statins was found to increase with age, male sex and higher SDI. A detailed analysis of individual risk factors is required to understand the differences.
To cite this abstract in AMA style:
Patel A, Jetanalin P, Galanter W, Adams E, CHANG H. Statin Use in Patients with Rheumatoid Arthritis (RA) and Osteoarthritis: Are RA Patients More Likely to Receive Statins? [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/statin-use-in-patients-with-rheumatoid-arthritis-ra-and-osteoarthritis-are-ra-patients-more-likely-to-receive-statins/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/statin-use-in-patients-with-rheumatoid-arthritis-ra-and-osteoarthritis-are-ra-patients-more-likely-to-receive-statins/