Session Information
Date: Tuesday, November 9, 2021
Title: Abstracts: RA – Diagnosis, Manifestations, & Outcomes II: Heart & Lung (1915–1918)
Session Type: Abstract Session
Session Time: 2:30PM-2:45PM
Background/Purpose: Increased levels of transforming growth factor β1 (TGF-β1) in the lung have been implicated in the pathogenesis of several fibrotic lung diseases, but their role in the lung in rheumatoid arthritis-associated interstitial lung disease (RA-ILD) has not been well studied. Evidence suggests that increased TGF-β1 production in the lung can be driven by IL-6 trans-signaling, which requires soluble IL-6 receptor (sIL-6R) complexed with IL-6 binding to membrane-bound gp130; this is in contrast to IL-6 classical-signaling that requires IL-6 binding to membrane-bound IL-6R (mIL-6R). Importantly, gp130, and not mIL-6R, is present on lung fibroblasts which play a key role in lung fibrosis. Also, mIL-6R is present on neutrophils and can be released to form sIL-6R during neutrophil extracellular trap (NET) formation. In this study, we sought to evaluate the relationships between TGF-β1, sIL-6R, NETs and the presence of ILD across a spectrum of patients with RA.
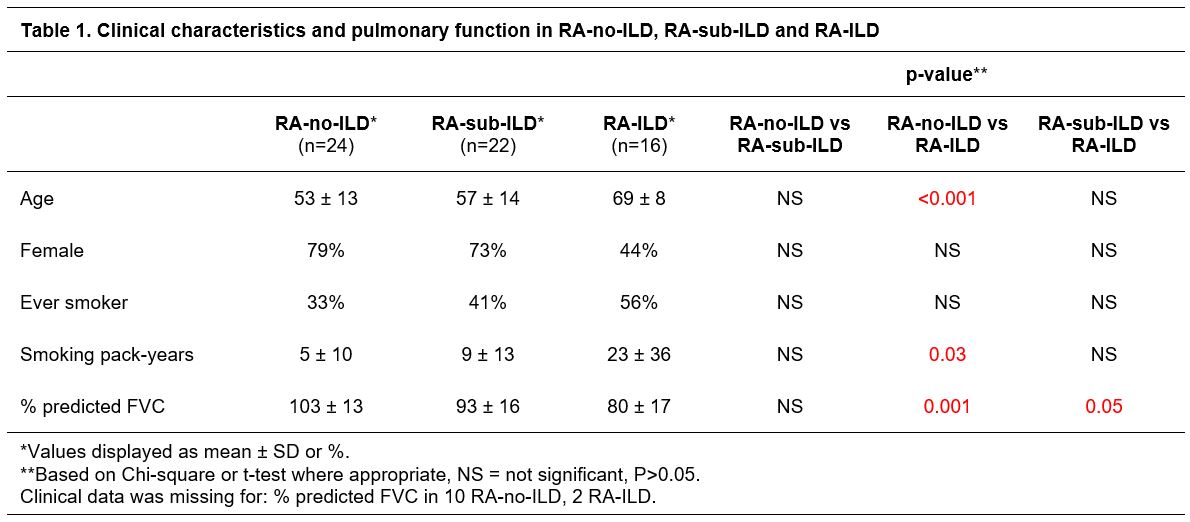
Methods: We included 16 RA patients with clinically significant ILD (RA-ILD), 22 RA patients with subclinical ILD defined as having parenchymal changes on lung high resolution computed tomography (HRCT) (i.e. fibrosis, traction bronchiectasis, reticulation and/or ground glass opacities) but no clinical diagnosis of ILD and normal pulmonary physiology (RA-sub-ILD), and 24 RA patients without ILD on HRCT (RA-no-ILD). All subjects underwent pulmonary function testing (PFT) and induced sputum was collected using hypertonic saline. Sputum was tested for TGF-β1 (Meso Scale Diagnostics) and sIL-6R (R&D Systems). Sputum IL-6 was measured in a subset of 8 RA-ILD, 4 RA-sub-ILD and 3 RA-no-ILD (Luminex) and sputum NET remnants in a subset of 11 RA-ILD and 3 RA-sub-ILD patients (sandwich ELISA for DNA-neutrophil elastase (NE) and DNA-citrullinated histone H3 (DNA-citH3)).
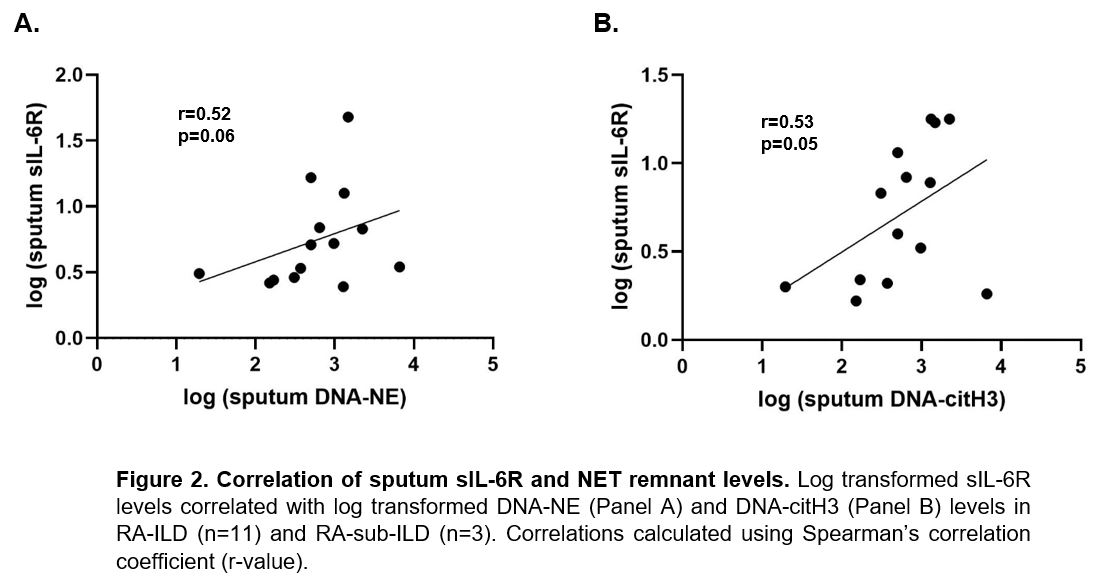
Results: Patient demographics are summarized in Table 1. Sputum TGF-β1 and sIL-6R levels were significantly higher in RA-sub-ILD and RA-ILD compared to RA-no-ILD (Figure 1A and 1B). In regression analyses adjusting for age and smoking, TGF-β1 and sIL-6R levels remained significantly associated with RA-sub-ILD and RA-ILD. Sputum TGF-β1 correlated with sIL-6R levels (Figure 1C) while there was no correlation between TGF-β1 and IL-6. In a subset of RA-sub-ILD and RA-ILD subjects, sputum NET remnants positively correlated with sputum sIL-6R levels (Figure 2A and 2B) but not TGF-β1 levels (p >0.20).
Conclusion: We found for the first time that sputum TGF-β1 and sIL-6R levels are increased in subclinical and clinically significant RA-ILD. The strong correlation between sputum TGF-β1 and sIL-6R along with the correlation between sputum sIL-6R and NET remnants suggest that increased TGF-β1 in the lung may be due to NET-associated increases in sIL-6R and subsequent IL-6 trans-signaling of lung fibroblasts. Future studies are needed to better understand the use of sputum TGF-β1 and sIL-6R as prognostic biomarkers in RA-ILD as well as mechanisms by which TGF-β1 production and IL-6 trans-signaling in the lung may contribute to RA-ILD.
To cite this abstract in AMA style:
Wilson T, Deane K, Lee J, Collora C, Feser M, Kaplan M, Solomon J, Demoruelle K. Sputum TGF-β1 Is Elevated in Subclinical and Clinically Significant Rheumatoid Arthritis-Associated Interstitial Lung Disease and Correlates with Soluble IL-6R Levels [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/sputum-tgf-%ce%b21-is-elevated-in-subclinical-and-clinically-significant-rheumatoid-arthritis-associated-interstitial-lung-disease-and-correlates-with-soluble-il-6r-levels/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sputum-tgf-%ce%b21-is-elevated-in-subclinical-and-clinically-significant-rheumatoid-arthritis-associated-interstitial-lung-disease-and-correlates-with-soluble-il-6r-levels/