Session Information
Date: Monday, November 14, 2022
Title: Abstracts: RA – Diagnosis, Manifestations, and Outcomes III: RA ILD
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Interstitial lung disease (ILD) is a well-recognized comorbidity in rheumatoid arthritis (RA) that contributes significantly to morbidity and mortality. ILD is diagnosed in up to 10% of RA patients but up to 40% of patients have subclinical lung parenchymal abnormalities without a clinical diagnosis of ILD. The mechanisms driving the development of RA-ILD including the progression of subclinical to established ILD remain poorly understood. Identifying sputum-based biomarkers, which are likely more reflective of the pathobiology in RA-ILD compared to blood-based biomarkers, may be more informative in characterizing the disease pathogenesis.
Methods: We evaluated 34 RA patients without ILD confirmed by high-resolution CT (HRCT) (RA-no-ILD), 18 RA patients with a clinical diagnosis of ILD as reviewed by a pulmonologist specializing in ILD (RA-ILD), and 24 RA patients with subclinical ILD defined as lung parenchymal abnormalities on HRCT but normal pulmonary physiology (RA-sub-ILD). Induced sputum was collected from all patients and HRCT and pulmonary function tests were completed within 3 months of sputum collection. Lung fibrosis was quantified by HRCT using data-driven textural analysis (DTA) fibrosis scores. Sputum supernatant was tested for levels of 31 cytokines/chemokines using multiplex assays (Meso Scale Discovery). A Random Forest (RForest) classifier model using sputum cytokines/chemokines was used to discriminate between RA-no-ILD and RA-ILD. DNA was extracted from participants with available serum to genotype for a single nucleotide polymorphism (rs35705950) within the promoter region of the MUC5B gene (Thermo Fischer) as the minor “T” allele has been shown to be one of the strongest risk factors for developing ILD in RA.
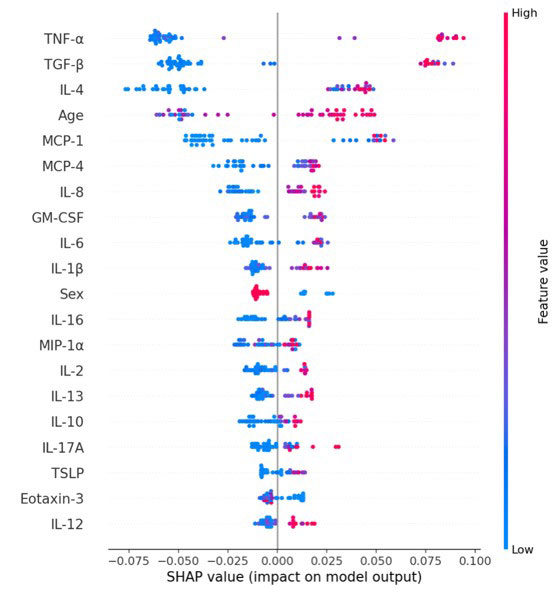
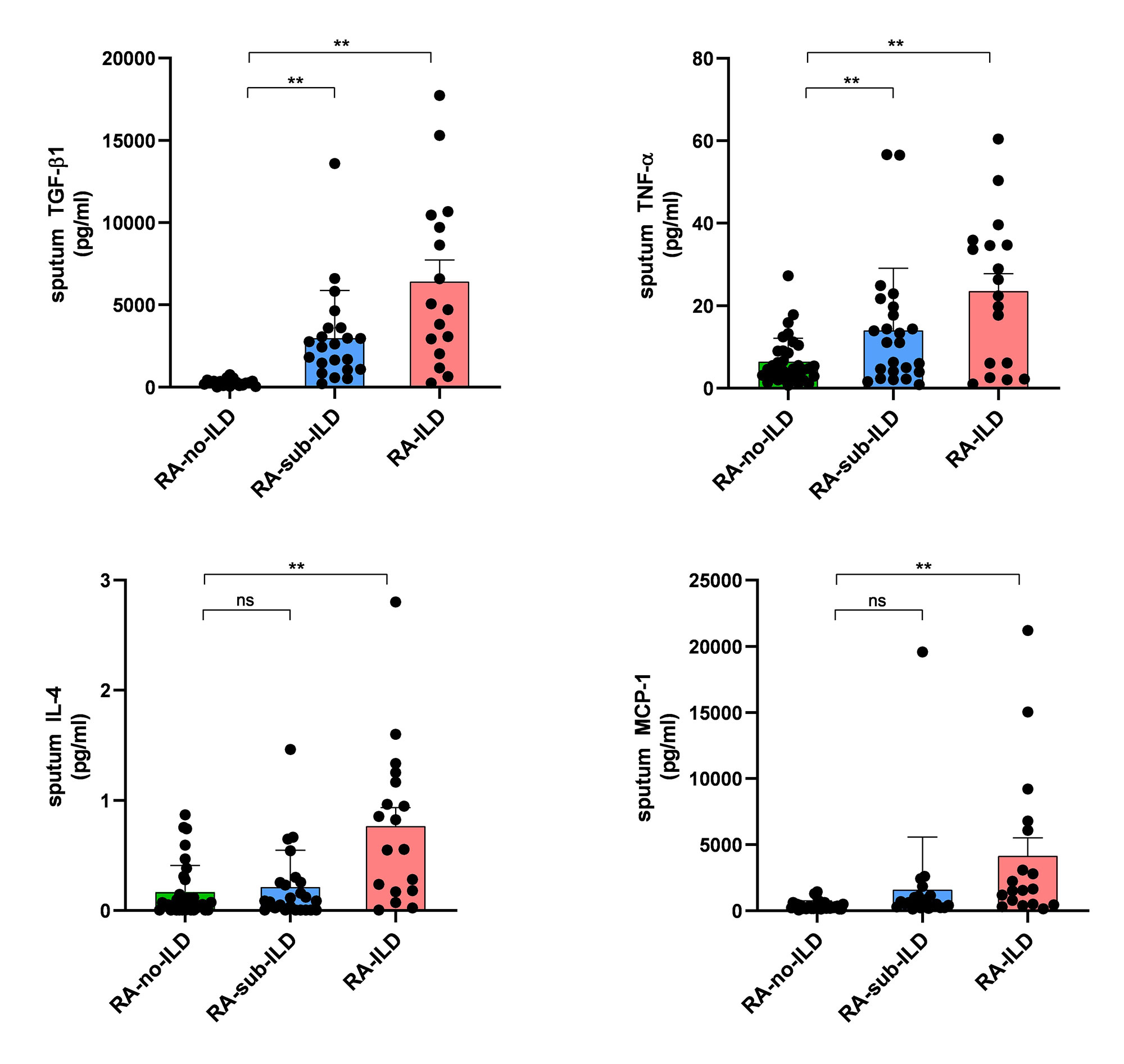
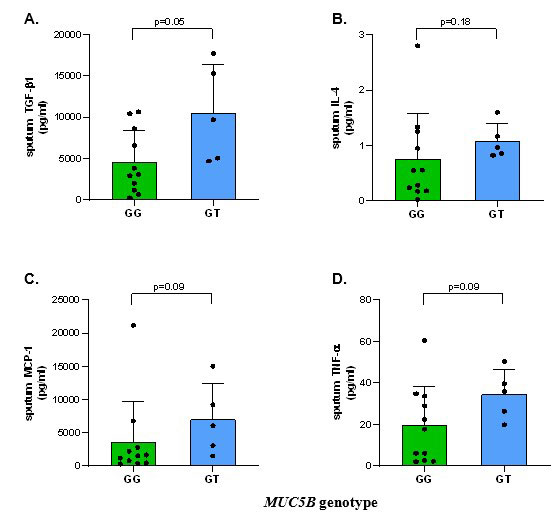
Results: Within the RForest model, transforming growth factor-beta 1 (TGF-β1), tumor necrosis factor-alpha (TNF-α), monocyte chemoattractant protein-1 (MCP-1), and interleukin-4 (IL-4) were the most impactful in classifying a patient as RA-ILD vs. RA-no-ILD (Figure 1); furthermore, these cytokines were significantly elevated in RA-ILD using multivariate regression models (Figure 2). TGF-β1 and TNF-α were also significantly elevated in RA-sub-ILD compared to RA-no-ILD (p=0.03 and p=0.05, respectively, Figure 2). TGF-β1 levels in RA-sub-ILD subjects were positively correlated with DTA fibrosis score. TNF-α levels in RA-ILD subjects were positively correlated with diffusion capacity of carbon monoxide (DLCO). Lastly, within RA-ILD, there was a trend toward higher cytokine levels in those with the at-risk MUC5B “T” allele compared to those homozygous for the wild type “G” allele (Figure 3).
Conclusion: We demonstrate that sputum levels of TGF-β1, TNF-α, MCP-1, and IL-4 are significantly elevated in RA-ILD and a portion of these cytokines are also increased in subclinical disease and correlated with lung physiology. In pilot testing, we also found a trend of higher sputum cytokine levels in RA-ILD subjects with the MUC5B promoter variant. Future studies are needed to better understand the role of these cytokines in ILD and specifically evaluate the influence of MUC5B genetics on cytokine generation in the lung and the development of RA-ILD.
To cite this abstract in AMA style:
Wilson T, Deane K, Dekermanjian J, Lee J, Feser M, Humphries S, Solomon J, Demoruelle K. Sputum Cytokines Are Elevated in Rheumatoid Arthritis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/sputum-cytokines-are-elevated-in-rheumatoid-arthritis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sputum-cytokines-are-elevated-in-rheumatoid-arthritis-associated-interstitial-lung-disease/