Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Spondyloarthritis (SpA) consists of clinically and genetically related but phenotypically distinct disorders, including ankylosing spondylitis, enteropathic arthritis, psoriatic arthritis, reactive arthritis, and enthesitis-related arthritis (subtype of juvenile idiopathic arthritis). The disease usually presents during adolescence and early adulthood where early recognition can reduce deformities and disability, improving quality of life for individuals with SpA. A growing body of literature has suggested the role of alteration in intestinal flora in pathogenesis of SpA, based on the significant overlap between SpA and inflammatory bowel disease (IBD). The most critical time period in gut flora formation is the neonatal period where the intestinal tract rapidly and dynamically transitions from sterility to extremely dense and diverse colonization. The determinants of gut microbiome during this period have not been established well with consistent findings. We hypothesized that individuals with SpA will have different neonatal environmental factors that may affect the gut microbiome compared with healthy individuals.
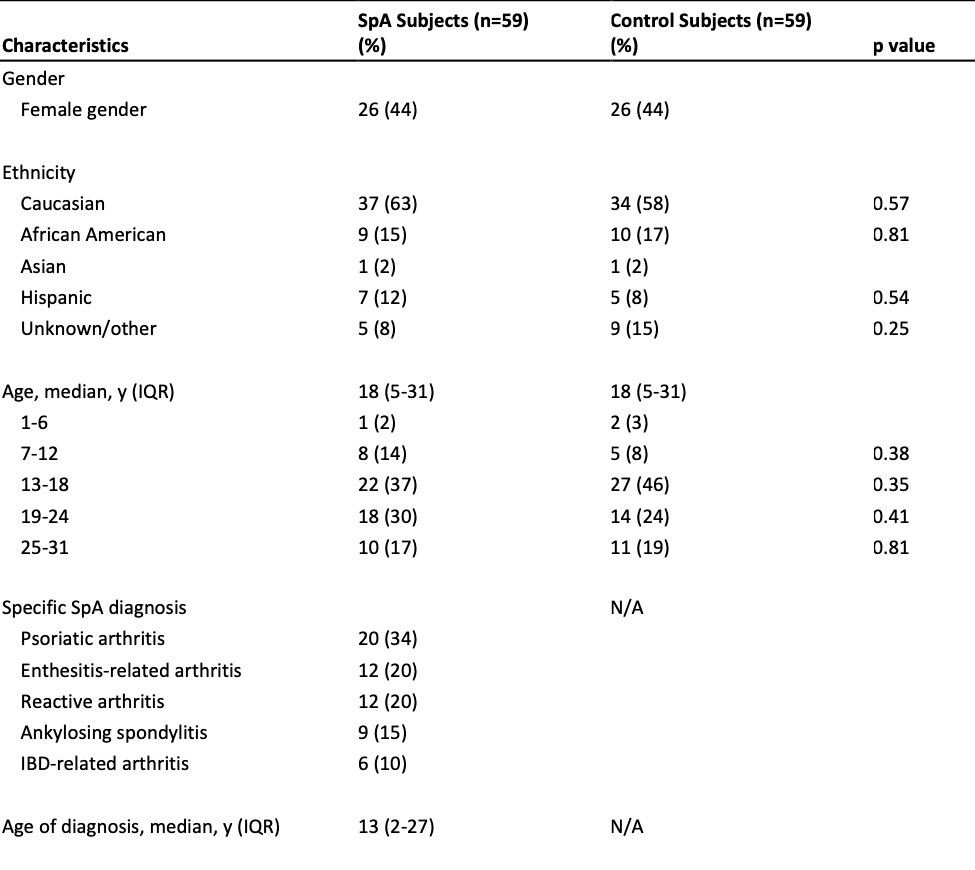
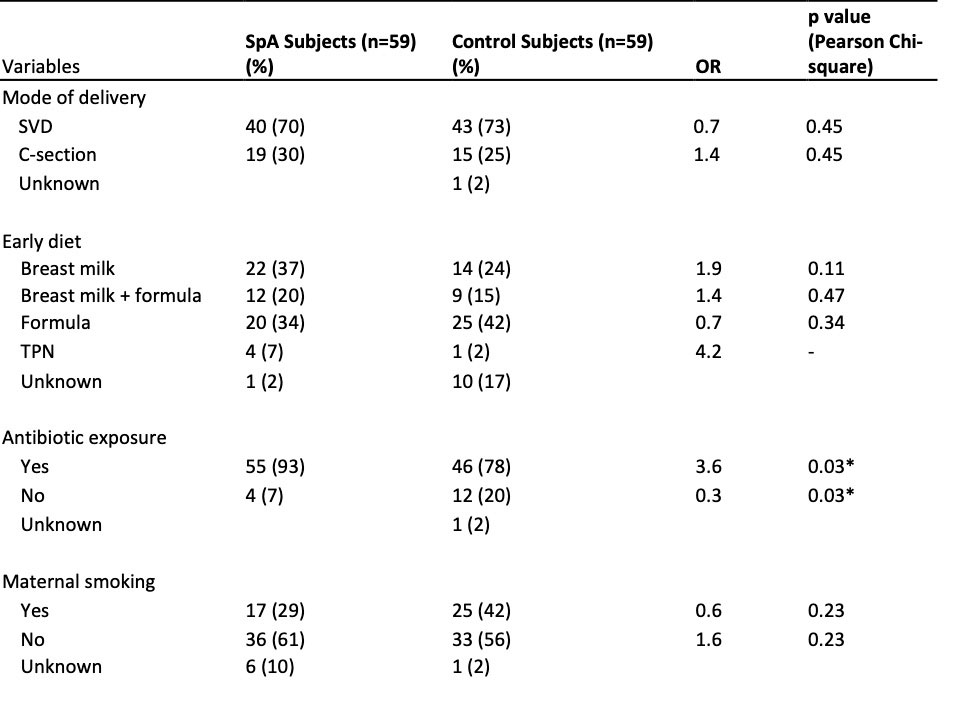
Methods: This was a retrospective, case-control study using electronic health records (EHR) data in a single Midwest academic health center. We examined perinatal factors known to affect neonatal gut microbiome–mode of delivery, early diet, antibiotic exposure, maternal smoking during perinatal period–in individuals with SpA diagnosed based on Assessment of Spondyloarthritis International Society (ASAS) criteria for axial and peripheral SpA as well as International League of Associations for Rheumatology (ILAR) criteria for enthesitis-related arthritis and juvenile psoriatic arthritis. Multiple logistic regression was used to examine the association between the neonatal factors affecting neonatal gut microbiome and SpA.
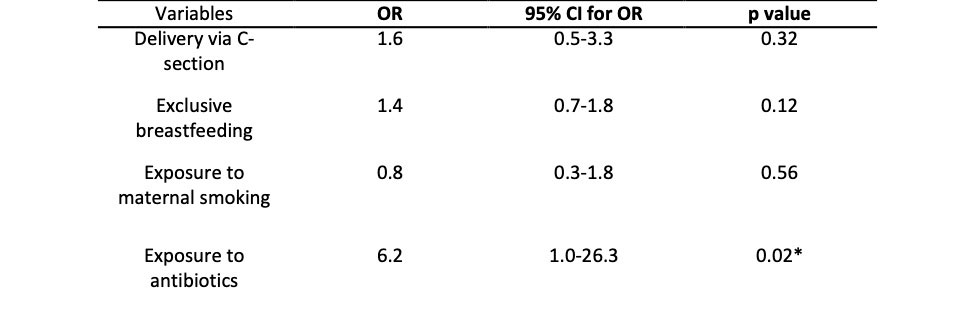
Results: A total of 59 individuals with SpA were identified and compared in neonatal factors with age- and gender-matched healthy controls. Higher proportion of individuals with SpA had antibiotic exposure preceding their diagnosis compared to healthy controls (93% vs 78% respectively, OR 3.6, p-value 0.03). Individuals with antibiotic exposure were 6.2 times more likely to develop SpA compared to those without antibiotic exposure (95% confidence interval [CI] 1.0-26.3, p-value 0.02), with statistical significance even after controlling for the effects of other neonatal factors. This association further increased with the greater number of antibiotic courses exposed. Mode of delivery, early diet, and maternal smoking during perinatal period did not show statistically significant association with SpA.
Conclusion: Antibiotic exposure may be associated with increased risk of developing SpA through its effect on perturbation and shaping of the gut microbiome during neonatal period and beyond. Out of all the perinatal factors studied and proposed to shape the gut microbiome during infancy, the effect of antibiotic exposure may outweigh others. Further studies elucidating the effect of environmental and therefore modifiable factors on the gut microbiome in SpA can guide new therapeutic approaches.
To cite this abstract in AMA style:
Um J, Einstadter D, Um M, Antonelli M. Spondyloarthritis and Neonatal Factors Affecting the Gut Microbiome [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/spondyloarthritis-and-neonatal-factors-affecting-the-gut-microbiome/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/spondyloarthritis-and-neonatal-factors-affecting-the-gut-microbiome/