Session Information
Date: Saturday, November 16, 2024
Title: Imaging of Rheumatic Diseases Poster I: Inflammatory Arthritis
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: In patients with inflammatory bowel disease (IBD), coexistence of spondyloarthritis (SpA), the most common extraintestinal manifestation, is associated with poor outcomes and impaired quality of life. Despite its significance, a considerable delay exists in diagnosing axial SpA in IBD patients. Therefore, the optimal treatment, which would target suppression of inflammation in all disease domains, may not be chosen.
This is the first study which aims to determine the prevalence and distribution of axial symptoms and MRI-detected involvement of the spine and sacroiliac joints (SIJs) in early IBD.
Methods: Newly diagnosed IBD patients from a prospective population-based cohort were consecutively included. Rheumatological interview, clinical and ultrasound evaluation of peripheral joints and entheses, and MRI assessment for SIJ and spine inflammatory and structural lesions were performed, using validated scoring methods and consensus definitions of axSpA [1-5].
Results: Of 110 included patients (ulcerative colitis: 70; Crohn’s disease: 40; mean age 42 years; 40% male), 81 had clinically active IBD. At the time of evaluation, only 4 patients received treatment with systemic glucocorticoid, and one received TNF-inhibitor. Nine patients were HLA-B27 positive. None were previously diagnosed with SpA. Back and/or buttock pain was reported by 48(44.9%) patients and 10(9.1%) had inflammatory back pain (Table 1). The axial symptoms were accompanied by peripheral joint and/or entheseal symptoms in 30(62.5 %). Peripheral arthritis and/or enthesitis was present in ̴half of the patients, in 56(52.3%) detected by clinical evaluation, and in 52(49.5 %) by ultrasound evaluation.
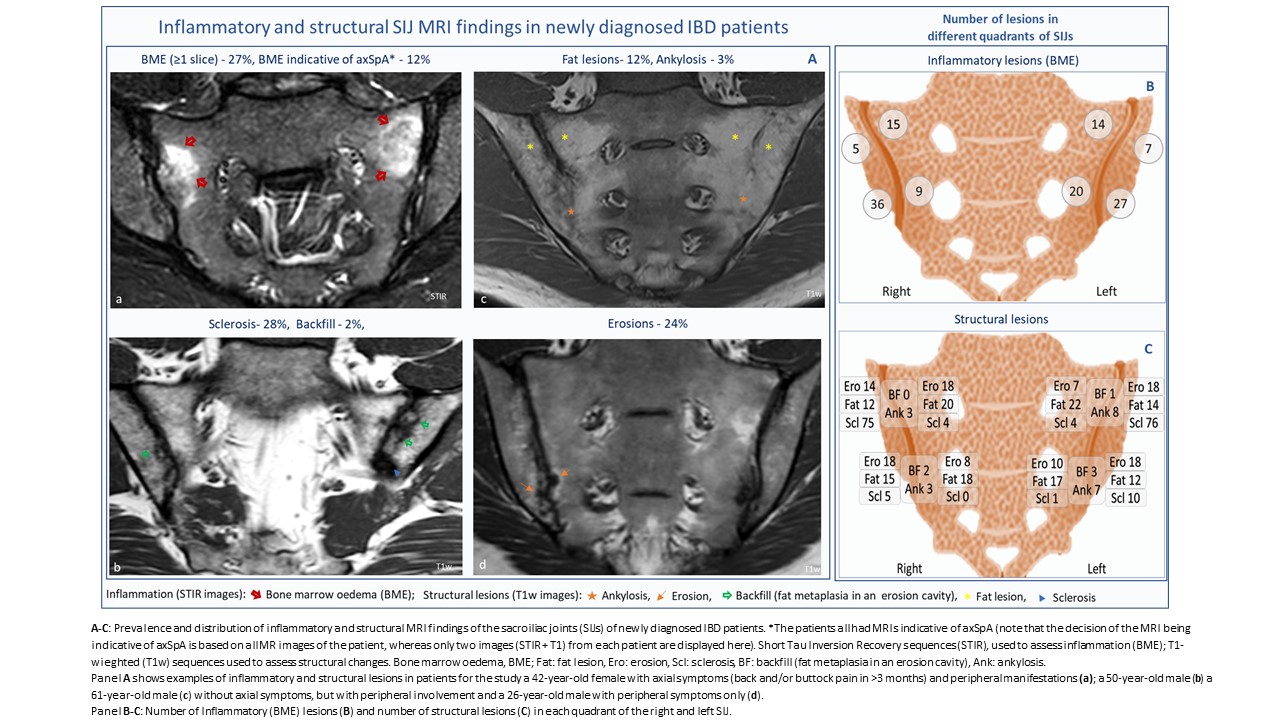
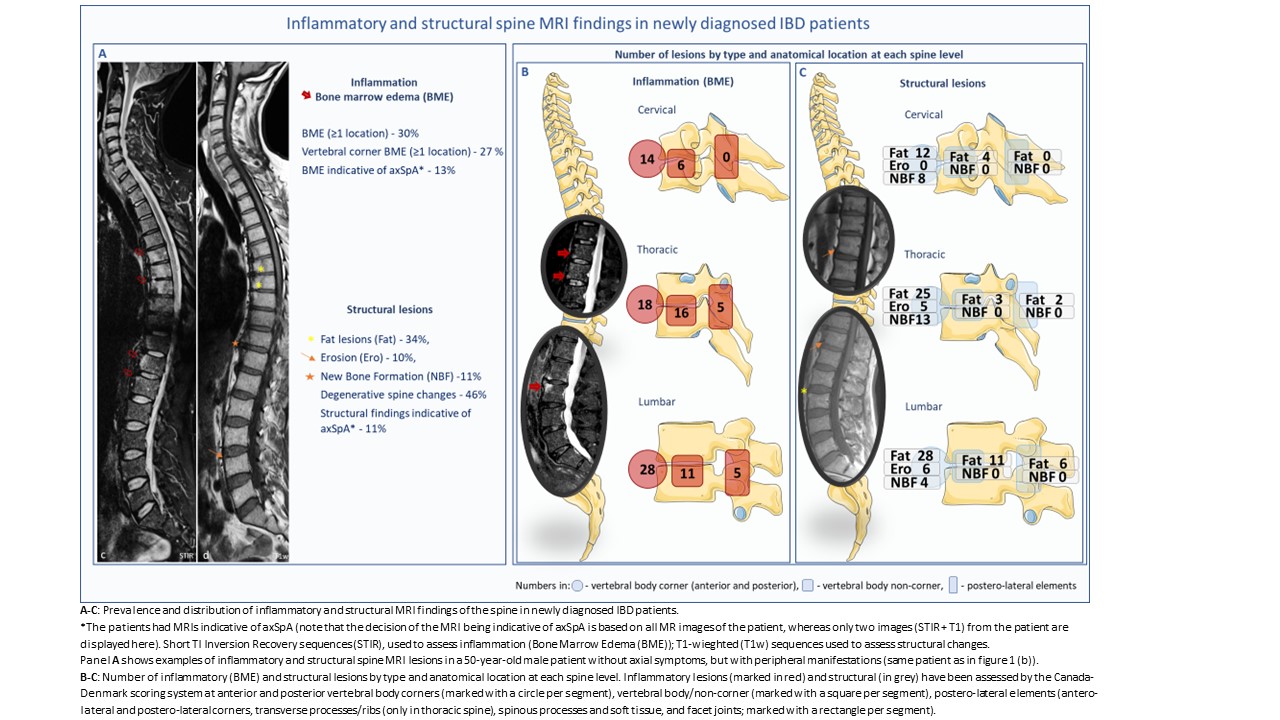
The prevalence and distribution of the inflammatory and structural MRI lesions of the SIJs and spine are shown in Figures 1-2. Seventeen (16.7%) patients had MRIs indicative of axSpA (Table 1). Ten (59%) of those patients had axial symptoms. The Assessment of SpondyloArthritis International Society (ASAS) definition of positive MRI for sacroiliitis was fulfilled in 12(11.8%) patients. The ASAS classification criteria for axSpA were met in 11(10%) cases and for axial or peripheral SpA in 47(43.5%) cases. Typical axSpA MRI findings were associated with peripheral joint and entheseal inflammation detected by ultrasound (Fisher’s test, p=0.04). There was no difference in clinical or imaging findings between patients with UC and CD, or between patients with active and inactive IBD.
Conclusion: Musculoskeletal involvement is frequent already at the time of IBD diagnosis and is often subclinical. One in six newly diagnosed IBD patients had findings indicative of axSpA on spine and SIJs MRI. Only ̴60% of these patients were symptomatic, suggesting that axSpA is underdiagnosed among IBD patients. Our results indicate that a multidisciplinary approach including imaging is required for an early detection of axial involvement, to enable appropriate treatment and prevent future structural damage and disability.
Ref.
- Maksymowych et al., Arthritis Rheum, 2005; 502-9
- Maksymowych, Arthritis Rheum, 2005; 703-9
- Maksymowych et al., J Rheumatol, 2015; 79-86
- Lambert et al., Ann Rheum Dis, 2016; 1958-1963
- Vladimirova et al., JCC 2024, Epub ahead of print
To cite this abstract in AMA style:
Vladimirova N, Møller J, Attauabi M, Madsen G, Terslev L, Wiell C, Fana V, Bay Hansen S, Siebner H, Seidelin J, Bentsen F, Gosvig K, Burisch J, Ostergaard M. Spine and Sacroiliac Joint Involvement in Newly Diagnosed Patients with Inflammatory Bowel Disease – Clinical and MRI Findings from a Population-Based Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/spine-and-sacroiliac-joint-involvement-in-newly-diagnosed-patients-with-inflammatory-bowel-disease-clinical-and-mri-findings-from-a-population-based-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/spine-and-sacroiliac-joint-involvement-in-newly-diagnosed-patients-with-inflammatory-bowel-disease-clinical-and-mri-findings-from-a-population-based-cohort-study/