Session Information
Date: Sunday, November 8, 2020
Title: Sjögren’s Syndrome Poster
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Smoking increases the risk of many rheumatic disease, including rheumatoid arthritis (RA). Previous studies have identified that current smoking might reduce the risk of primary Sjӧgren’s syndrome (SS), but it remains unknown whether smoking is positively or negatively associated with SS among RA patients. The objective of this cross-sectional study was to examine the relationship between smoking and RA-SS overlap in a large RA cohort.
Methods: Electronic health records from a rural, population-based cohort were screened for RA cohort eligibility. Inclusion criteria include age ≥18 years, at least two RA diagnosis codes from a rheumatologist on distinct dates within a two year period or positive rheumatoid factor or ant-CCP antibody between 1/1/2005 and 12/31/2018. Index date was defined by the first RA diagnosis code. The baseline period for evaluation of comorbidities and medication use began twelve months before the index date. The independent variable of smoking status was defined as never, current, or past (quit) smoker at or before the index date. The dependent variable of SS was defined by ICD 9 code 710.2. Descriptive statistics were performed using chi square for categorical and unpaired student’s t-test for continuous variables. Multivariable logistic regression was performed to determine odds ratios (ORs) of SS as the primary outcome by smoking status. Models were adjusted for age, sex, and race.
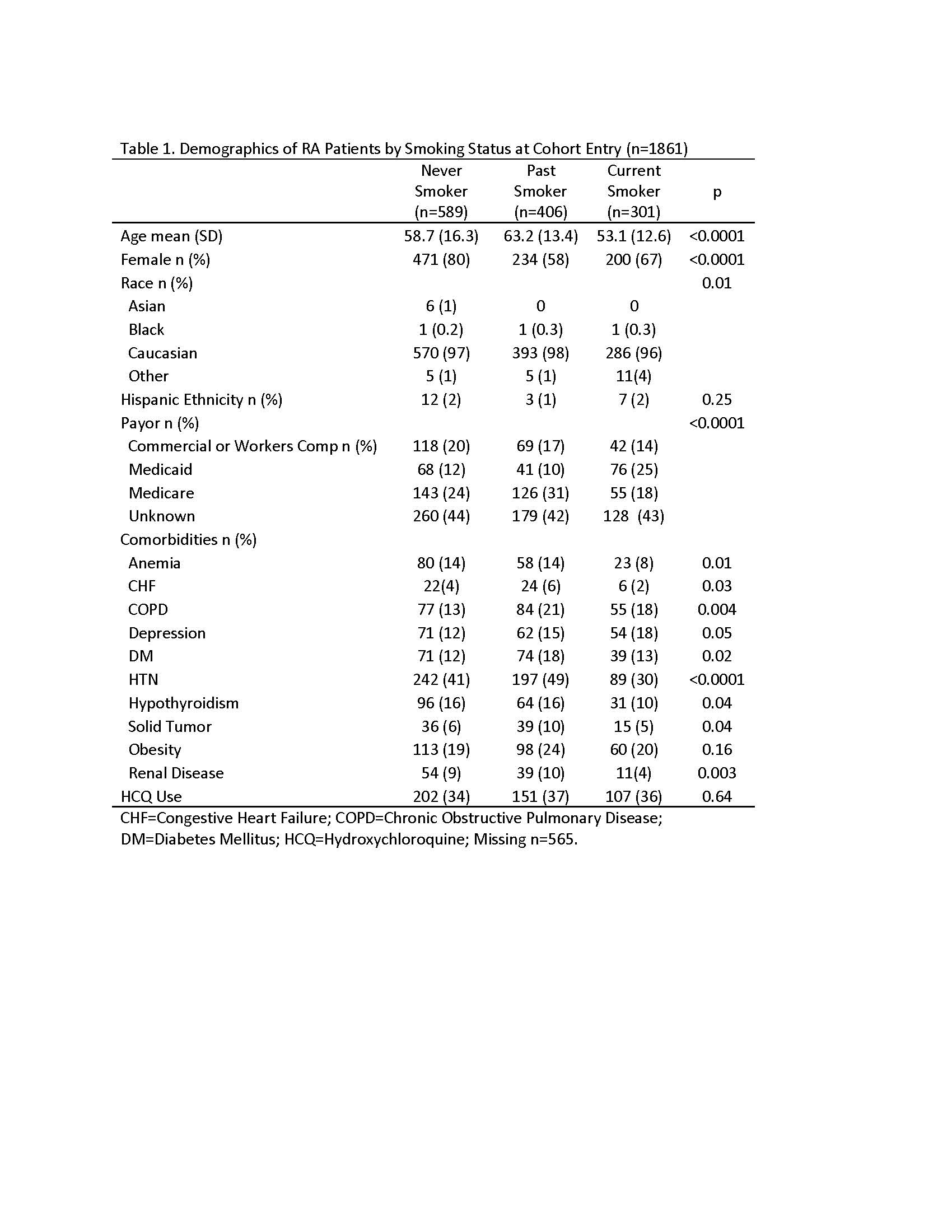
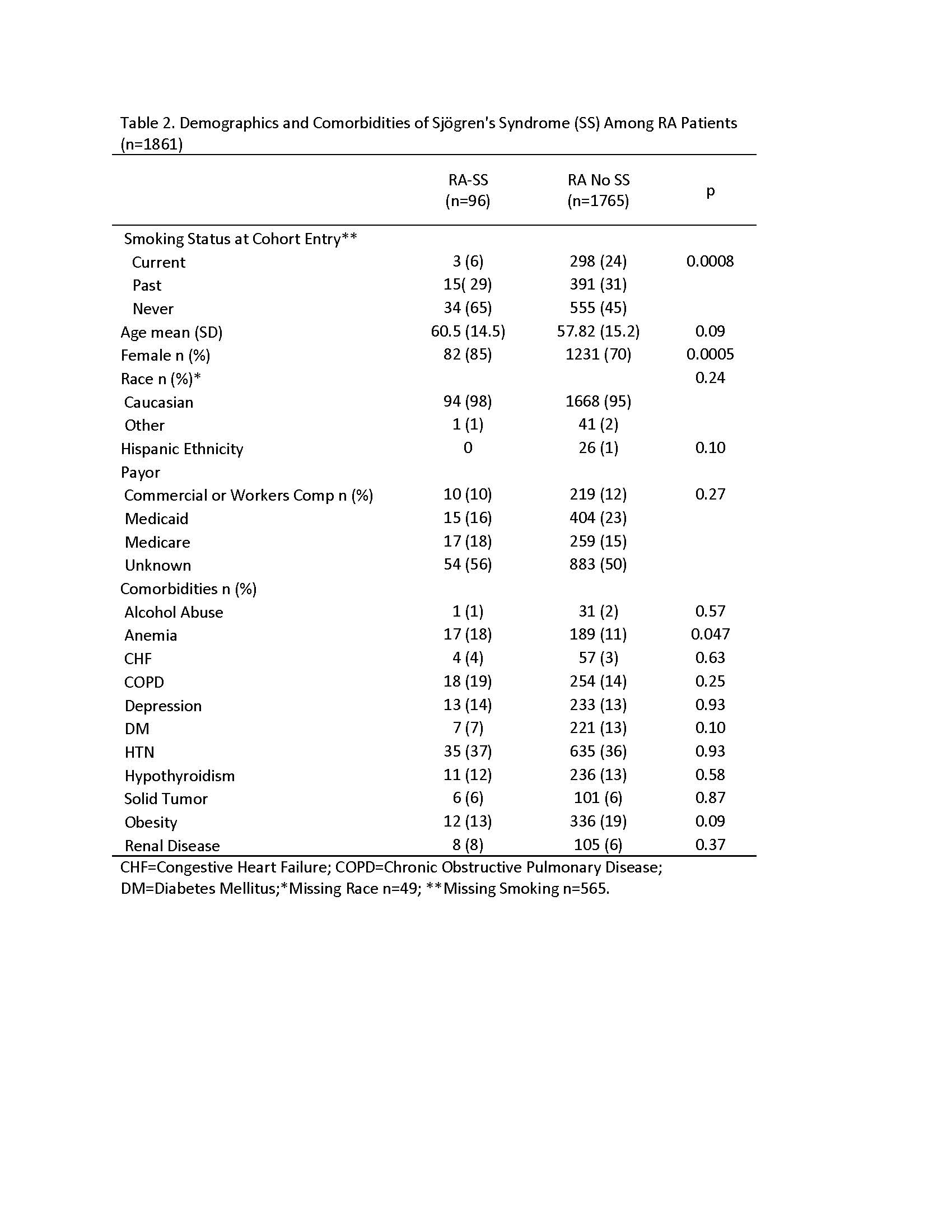
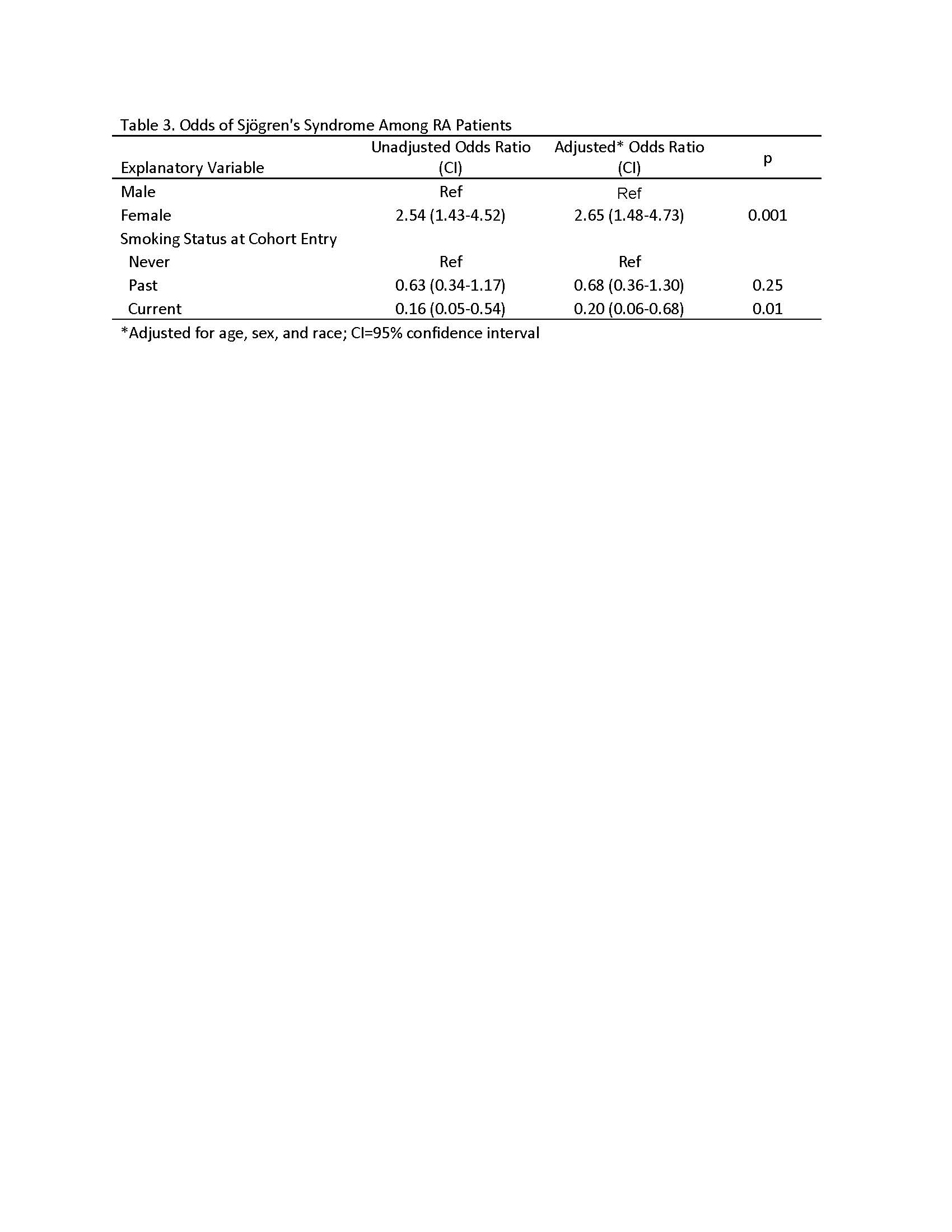
Results: Among 1861 patients with RA identified for cohort inclusion, 1296 patients had a reported smoking status available. Current smokers were younger and had lower female predominance than never and past smokers (Table 1). Fewer current smokers had anemia, congestive heart failure, hypertension, hypothyroidism, and renal disease. Descriptive analysis of RA patients with or without SS revealed that SS patients were more likely to be female and less likely to be anemic or smoke (Table 2). Adjusted OR of female sex was positively associated with SS (OR 2.56 [95% Confidence Interval (CI) 1.48-4.73]; Table 3). Current smoking was negatively associated with SS (OR 0.2 [95% CI 0.06-0.68]). Because data on smoking before cohort entry were missing for 565 patients, we repeated analysis on smoking status of patients captured before cohort exit (38 patients missing) and reproduced these results (data not shown).
Conclusion: We report for the first time that RA patients who smoke had 80% lower odds of SS. Previously, studies have shown reduced risk of primary SS in current smokers, supporting our findings. We found female sex in RA had a greater than 2.5 fold association with SS. Our data suggest a negative correlation between smoking and SS among RA patients. Our cross-sectional observational study cannot exclude reverse causality of quitting smoking with SS symptoms. Future studies should prospectively examine pack year dose relationships with overlap RA-SS incidence to further examine risk reduction and causality.
To cite this abstract in AMA style:
McCoy S, Bartels C. Smoking Might Reduce Odds of Sjӧgren’s Syndrome Among Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/smoking-might-reduce-odds-of-sj%d3%a7grens-syndrome-among-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/smoking-might-reduce-odds-of-sj%d3%a7grens-syndrome-among-rheumatoid-arthritis-patients/