Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: While a handful of clinical risk factors for the development of inflammatory diseases have been identified, to date, no studies have compared risk factors across multiple inflammatory diseases. The objective of this study was to compare the strength of association of selected potential risk factors for the development of psoriasis, PsA, RA, and AS.
Methods: We performed a series of case-control studies in The Health Improvement Network, a general practitioner database in the United Kingdom. Data between 1994-2015 were included. We identified patients with at least one code for PsA, RA, AS, or psoriasis using validated code lists and matched them to up to ten controls from the general population without these diseases based on age (within 2.5 years), sex, practice and year of diagnosis (controls were required to be in the practice on the diagnosis date and were assigned the same ‘diagnosis date’). We began with an extensive code list of over 100 potential risk factors including common comorbidities, infections, trauma, and a limited number of medications (e.g., statins). Potential risk factors were assessed from the time of enrollment into a THIN practice until the end of the observation period, end of enrollment, or death. Hypothesized risk factors with a prevalence of ≥1% were included in the final models and tables. Univariable logistic regression was used to screen risk factors for association with the disease of interest. Multiple testing was accounted for by setting a p-value of 0.02 as the level of statistical significance. Finally, a multivariable logistic regression model was constructed for each disease using the significant risk factors, stratified by sex.
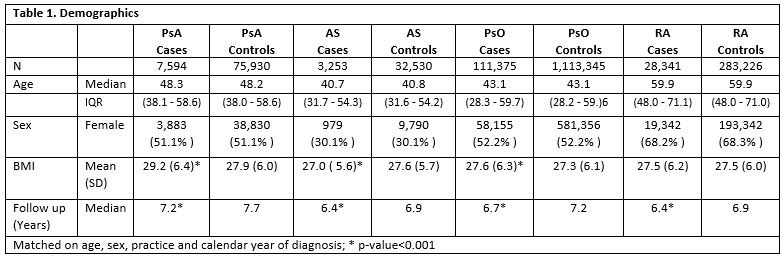
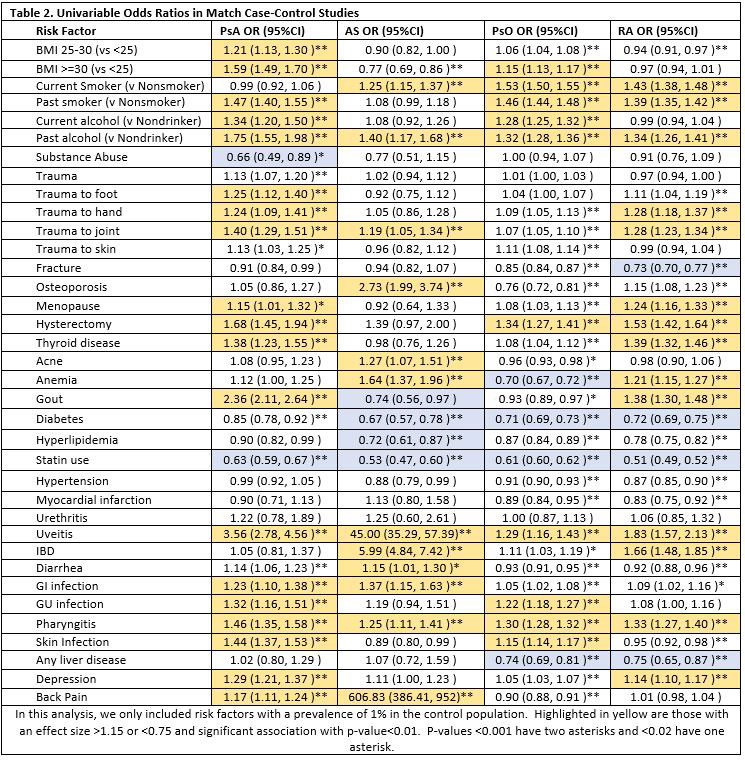
Results: Demographics of the patient population are shown in Table 1: 7,594 incident PsA cases, 3, 253 incident AS cases, 111,375 incident psoriasis cases, and 28,341 incident RA cases were identified and matched to 75,930, 32,530, 1,113,345, and 282,226 controls respectively. Median age at diagnosis was 48.3 (IQR 38-59), 40.7 (31-54), 43.1 (31-54), and 59.9 (48-71) respectively. Sex was balanced in psoriasis and PsA but more female in RA (68%) and more male in AS (70%). Mean follow up time ranged from 6.4-7.2 years and was slightly longer among controls. In univariable analyses (Table 2), previously identified risk factors in PsA were replicated including obesity, uveitis, and trauma. Smoking was identified as a risk factor in RA as previously described. There were some similar risk factors across all 4 diseases including a positive association between pharyngitis, IBD and uveitis (strongest for AS and PsA) and a similarly strong protective effect of statins. Skin infections were associated with PsA and psoriasis, skin trauma with psoriasis and joint trauma with PsA. Diarrheal infections were associated with PsA and AS. Most risk factors maintained statistical significance in the multivariable models though final models differed slightly by sex.
Conclusion: This set of parallel case-control studies identifies differences between PsA, psoriasis, AS and RA that supports the previous theories of pathophysiologic triggers related to these diseases but also demonstrates some commonalities between diseases.
To cite this abstract in AMA style:
Ogdie A, Wang X, Love T, Thrastardottir T, Dubreuil M, Gelfand J. Shared and Differing Risk Factors for PsA, Psoriasis, AS, and RA: A Series of Case-control Studies [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/shared-and-differing-risk-factors-for-psa-psoriasis-as-and-ra-a-series-of-case-control-studies/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/shared-and-differing-risk-factors-for-psa-psoriasis-as-and-ra-a-series-of-case-control-studies/