Session Information
Date: Saturday, November 6, 2021
Title: Sjögren's Syndrome – Basic & Clinical Science Poster (0296–0322)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Sjӧgren’s syndrome (SS) is the most female predominant systemic autoimmune disease, with peak onset around perimenopause. Estrogen appears to protect against SS, but prior studies lack details on surgical interventions and timing or type of exogenous hormone exposure. The purpose of this study was to determine how specific endogenous and exogenous hormone exposures contribute to SS Risk.
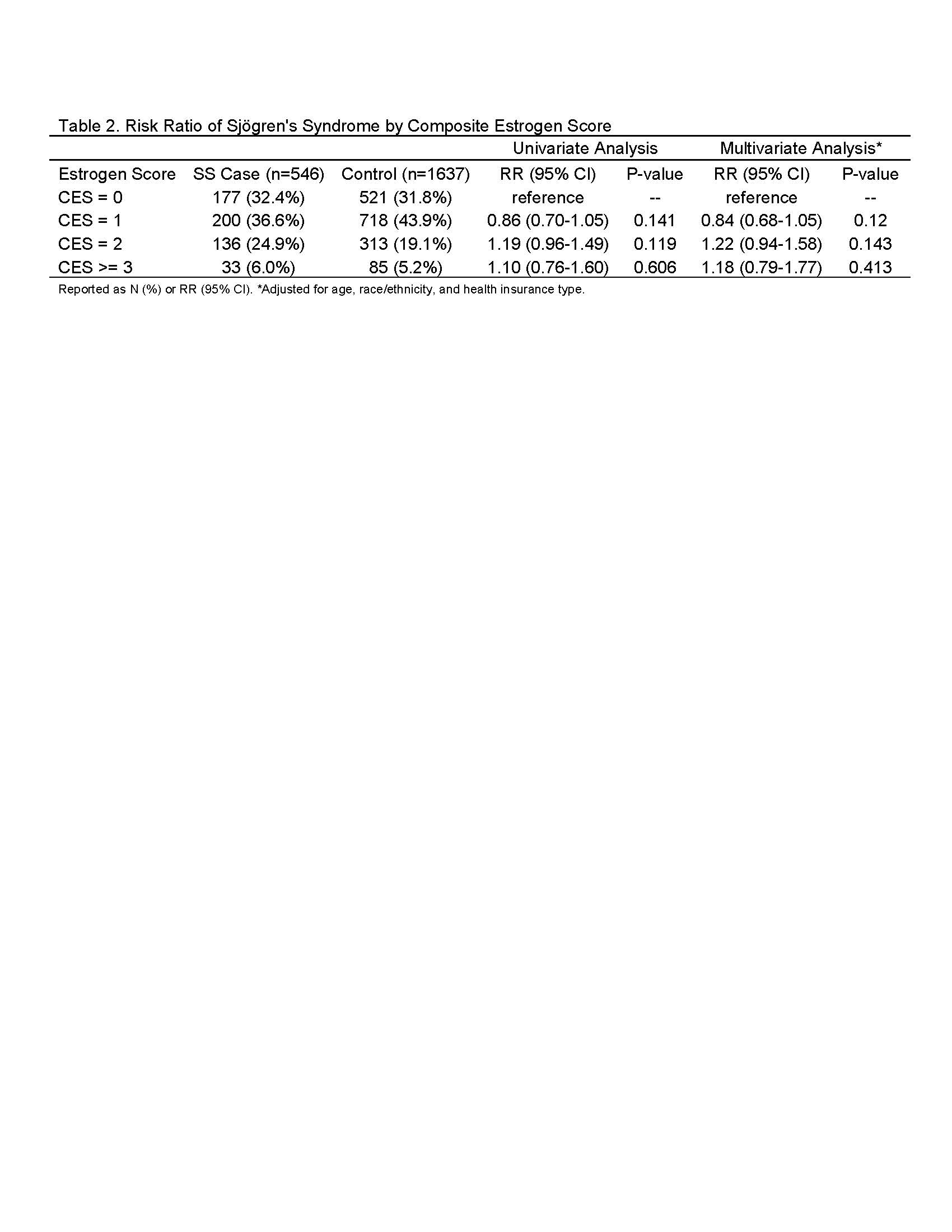
Methods: We performed a retrospective case-control study of adult women, nested within a defined population of Marshfield Clinic Health System (MCHS) patients in north-central Wisconsin. SS cases included patients with one SS diagnosis by a rheumatology provider or two SS diagnoses > 4 weeks apart from a non-rheumatology provider. Those with overlapping autoimmune diseases were excluded. Three controls were included for each SS case and were matched on age. We calculated a composite estrogen score (CES) for each patient, with one point for: 1) body mass index (BMI) ≥30 kg/m2, 2) menopause ≥55 years, 3) hormone replacement therapy >90 days, and 4) hysterectomy, which was considered a marker of high estrogen because hysterectomy is most often performed for fibroids and post-surgical management often includes exogenous hormones. Risk ratios for SS were reported, adjusted for age, race/ethnicity, and health insurance.
Results: There were 546 SS cases and 1,637 age-matched controls. The distribution of CES was 0 (n= 698 (32%)), 1 (n= 918 (42%)), 2 (n= 449 (21%)), and >= 3 (n=118 (5%)) (Table 1). Age, race, and ethnicity were similar between CES groups but health insurance differed. CES was not significantly associated with SS in adjusted models (Table 2). As outlined in Figure 1, the top three individual hormone exposures that were independently associated with SS included hirsutism (RR 2.42 [95% CI 1.32-4.43]), ovarian cysts, (2.12 [1.48-3.04]) and exogenous hormone replacement therapy (1.84 [1.20-2.81]). High BMI (0.62 [0.50-0.77]) and aromatase inhibitor use (0.25 [0.07-0.83]) appeared to be protective against SS.
Conclusion: Higher CES did not result in greater SS risk in this study, but several novel individual SS risk factors were observed, most notably hirsutism and ovarian cysts, which are associated with high androgen and lower estrogen excess. In contrast, high BMI, which is associated with higher levels of peripherally produced estrogen and lower androgen, was associated with lower SS risk. Aromatase inhibitor or SERM use also appeared protective, potentially representing confounding by indication because higher levels of estrogen are associated with breast cancer. These data suggest that the influence of sex hormones on SS pathogenesis may be more complex than prior studies have indicated; SS risk is potentially dependent on androgen-to-estrogen ratios. Further prospective studies are needed to confirm these findings.
To cite this abstract in AMA style:
McCoy S, Bartels C, Hetzel S, VanWormer J. Sex Hormones and Risk of Sjögren’s Syndrome: Hypothesis Generating Findings Implicating Androgen and Estrogen Ratios [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/sex-hormones-and-risk-of-sjogrens-syndrome-hypothesis-generating-findings-implicating-androgen-and-estrogen-ratios/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-hormones-and-risk-of-sjogrens-syndrome-hypothesis-generating-findings-implicating-androgen-and-estrogen-ratios/