Session Information
Date: Tuesday, November 15, 2016
Title: Metabolic and Crystal Arthropathies - Poster II: Epidemiology and Mechanisms of Disease
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Both serum urate (sUA) and endothelial dysfunction have been associated with hypertension and cardiovascular disease. Increasing sUA level has been associated with endothelial dysfunction and higher inflammatory markers (e.g., high sensitivity c –reactive protein [hsCRP]). To date, however, few studies have examined the relationship between sUA, endothelial dysfunction, and blood pressure (BP) including young and largely healthy individuals. Objectives: To determine whether there is an association between higher sUA, endothelial dysfunction as measured by flow-mediated dilation (FMD), and BP in young adults.
Methods: We conducted a cross-sectional analysis of baseline data for consecutively enrolled individuals (age 18 – 40 years). Inclusion criteria were: baseline systolic BP (SBP) ≥ 120 and <160 mmHg or diastolic BP (DBP) ≥ 80 and < 100 mmHg, and sUA ≥ 5.0 mg/dL for men or ≥ 4.0 mg/dL for women. Clinic SBP and DBP, 24- hours ambulatory BP monitoring (ABPM), hsCRP, and sUA level were obtained. Associations between sUA, endothelial dysfunction measured by FMD, and ABPM variables were evaluated using a general linear model. Adjustments for age, gender, race, and BMI were applied after significant univariate results. Data reported are mean +standard deviation (SD).
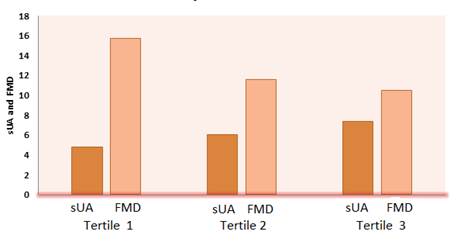
Results: There were 69 participants included in the analysis. Participants recruited had a mean age of 29.0 ± 6.9 years, 30 % were female, 43 % African-Americans, mean BMI was 29.0 ± 6.0 kg/m², and mean sUA was 5.9 ± 1.1 mg/dL (range from 3.9 to 8.5 mg/dL). We found no significant cross-sectional associations between sUA, FMD, and BP variables assessed by ABPM (Table). Participants in the upper tertile of sUA had significantly more endothelial dysfunction as measured by FMD than those in the lower tertiles (Figure). However, this difference was no longer significant after multivariable adjustment age, gender, race, and BMI.
Conclusion: In this cross-sectional analysis of young adults, there was no evidence to support an association between sUA levels and endothelial dysfunction or BP. Endothelial dysfunction or BP might be associated with changes in sUA when measured longitudinally in individuals, but not when measured cross-sectionally in populations. Larger studies will be needed to confirm these results. Table. Cross-sectional correlation between sUA, FMD, and Ambulatory Blood Pressure parameters
| Parameters | r | p-value |
| sUA and FMD | -0.19 | 0.15 |
| sUA and SBP | -0.02 | 0.85 |
| sUA and DBP | -0.07 | 0.61 |
| sUA and MAP | -0.02 | 0.86 |
sUA: serum uric acid, SBP: systolic blood pressure, DBP: diastolic blood pressure, MAP: mean arterial blood pressure, FMD: flow-mediated dilation Figure. Tertiles of sUA and FMD unadjusted correlation
The p for trend for FMD across SUA tertiles is p = 0.006
To cite this abstract in AMA style:
Saddekni MB, Saag KG, Dudenbostel T, Oparil S, Calhoun DA, Feig DI, Muntner PM, Redden DT, Foster PJ, Rahn EJ, Biggers SR, Li P, Gaffo AL. Serum Urate and Its Association with Endothelial Dysfunction in Young Adults [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/serum-urate-and-its-association-with-endothelial-dysfunction-in-young-adults/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-urate-and-its-association-with-endothelial-dysfunction-in-young-adults/