Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have a 2-3-fold increased risk of cardiovascular events. A major risk factor for this is hypertension. We previously demonstrated that downstream products of oxidative stress, isolevuglandins (isoLGs) promote hypertension and autoimmunity in SLE. IsoLGs covalently bind to lysine residues, leading to increased tissue damage, inflammation, and formation of autoantigens. The purpose of this study is to determine if anti-isoLG IgG antibodies are increased in patients with SLE and associated with disease activity and blood pressure (BP).
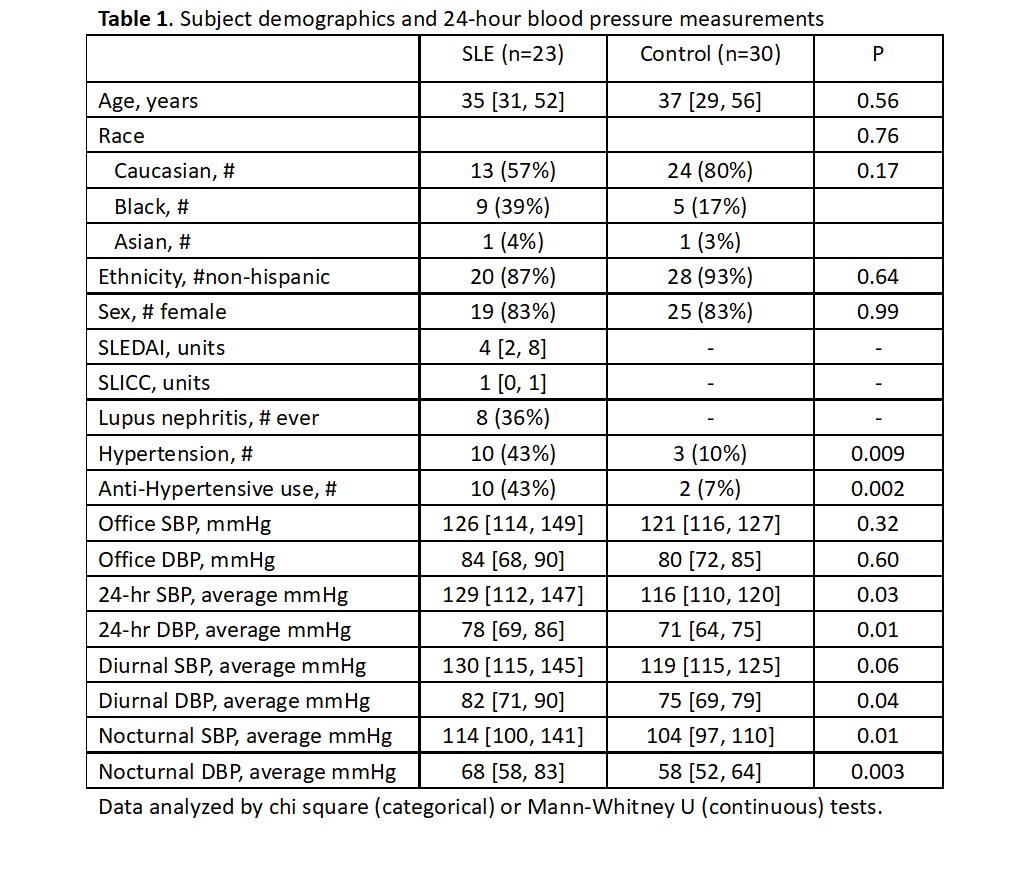
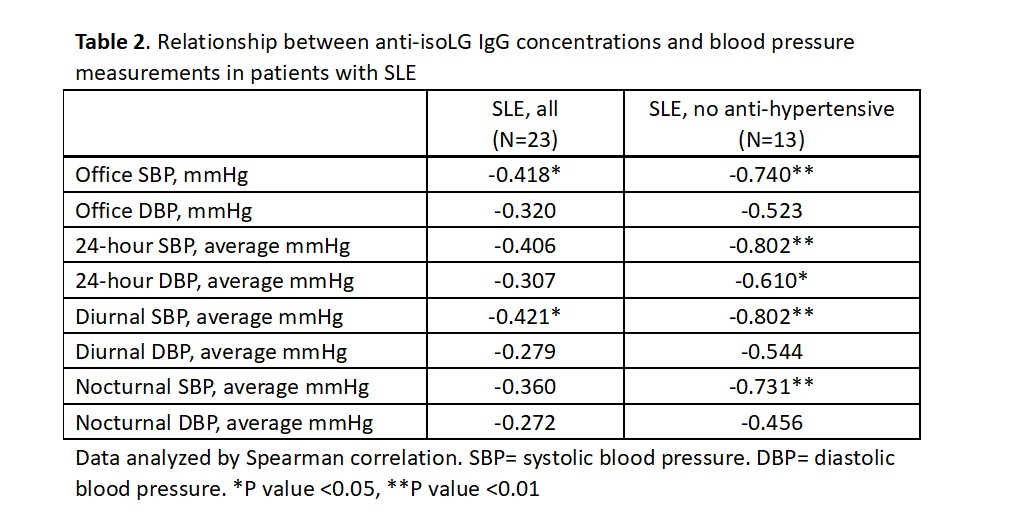
Methods: This cross-sectional study included 23 SLE and 30 control subjects. Subjects wore an ambulatory BP monitor for 24 hours with diurnal measurements every 15-30 minutes and nocturnal measurements every 30 minutes. Serum-isoLG IgG antibody concentrations were measured using a sandwich ELISA as previously published. One SLE serum sample was used on all plates to normalize for plate-to-plate variability. Data were compared by chi square (categorical) or Mann-Whitney U (continuous) tests. Correlation was conducted by Spearman rho and linear regression analysis with anti-isoLG IgG antibody concentrations log-transformed to normalize residuals.
Results: Patients with SLE and control subjects were of similar age, race, and sex. Disease activity in SLE patients was low to moderate (mean SLEDAI=4). Most 24-hour BP parameters were significantly elevated in SLE versus control subjects (Table 1). Serum anti-isoLG IgG antibody concentrations were increased in SLE (median [interquartile range]: 1.30 units [0.93, 1.70 units]) versus control subjects (0.91 units [0.73, 1.28 units], P=0.007; Figure 1). Anti-isoLG IgG antibody concentrations were significantly inversely associated with office and diurnal systolic BP (Table 2) in patients with SLE but were not significantly associated with BP in control subjects or disease activity and damage in SLE (SLEDAI: rho=0.156, C4: rho=-0.320, SLICC: rho=0.338). SLE patients not taking anti-hypertensive drugs were examined separately due to impact of the anti-hypertensives on BP and anti-isoLG IgG antibody concentrations were strongly significantly inversely associated with office and 24-hour BP measurements (Table 2). For example, every 20% increase in anti-isoLG IgG concentration was associated with a 10 mmHg decrease in 24-hour systolic BP, P=0.004. This remained significant after adjustment for age (P=0.03).
Conclusion: Serum concentrations of anti-isoLG IgG antibodies are increased in SLE versus control subjects. Anti-isoLG IgG antibody concentrations were inversely associated with 24-hour BP measurements. Given prior mechanistic studies demonstrating that cellular isoLGs promote hypertension, it is possible that in SLE, isoLG antibodies could help clear these hypertension-inducing antigens. Future work will further evaluate this mechanism and the role of anti-isoLG IgG antibodies as markers of BP and cardiovascular risk.
To cite this abstract in AMA style:
Phothisane A, Shaik S, Wu Q, Posey O, Davies S, Krishnan J, Patrick D, Stein C, Ormseth M. Serum Isolevuglandin IgG Antibody Concentrations Are Increased in Patients with Systemic Lupus Erythematosus versus Control Subjects and Associated with Lower 24-hour Blood Pressure [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/serum-isolevuglandin-igg-antibody-concentrations-are-increased-in-patients-with-systemic-lupus-erythematosus-versus-control-subjects-and-associated-with-lower-24-hour-blood-pressure/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-isolevuglandin-igg-antibody-concentrations-are-increased-in-patients-with-systemic-lupus-erythematosus-versus-control-subjects-and-associated-with-lower-24-hour-blood-pressure/