Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: SLE is characterized by increased type I IFN signature in the blood and immune cells. Traditionally, type I IFN signature is measured by gene expression analysis however it is difficult to compute in routine clinical practice. IFN alpha levels are very low and need a highly sensitive assay for its measurement, thus we aimed to look at proteins affected by IFN-alpha like galectin-9 and CXCL-10 as markers of SLE activity as well as for lupus nephritis.
Methods: Patients with SLE (fulfilling SLICC criteria) were included and clinical parameters recorded. They were divided based on renal involvement and disease activity into—active (SLEDAI>4) renal, active non-renal and inactive subgroups. 20 healthy controls (HC) were also included. Serum and urine galectin-9 and CXCL-10 levels were measured by ELISA. Urine galectin-9 and CXCL-10 were normalized with spot urine creatinine values. Follow-up serum and urine galectin-9 levels were measured for those in the active renal group at six-months. Non-parametric test like Kruskal Wallis test, Spearman’s correlation coefficient, and ROC curve analysis were used.
Results: 97 patients with SLE (26 years; 89 females) were categorized into active renal disease (35), inactive disease (32) and active non-renal disease (30). 20 HC (25 years; 15 females) were enrolled.Themedian duration of disease was 24 months (6-48)and SLEDAI 2K was 9 (2-15).
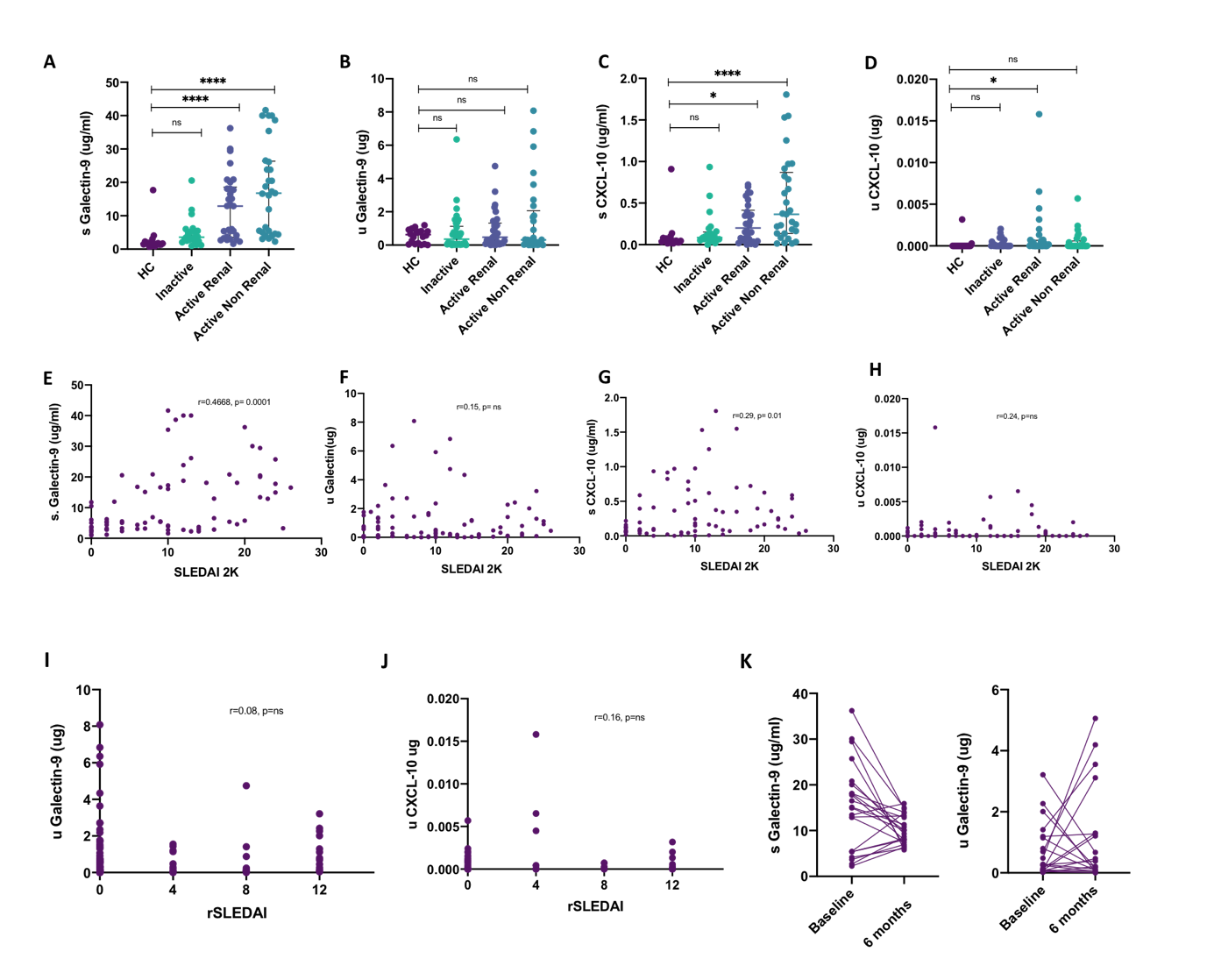
Patients with SLE had higher serum galectin-9 (5.652 vs 1.702 ug/ml, p=0.0001) but not urine galectin-9 (0.538 vs 0.317 ug, p=0.7) levels as compared to HC. Serum galectin-9 but not urine galectin-9 was higher in patients with active as compared to inactive lupus (12.912 in active renal, 16.777 in active non-renal vs 3.565 ug/ml, p=0.04 and 0.005). There was no significant difference in serum or urine galectin-9 between active renal and active non-renal disease.
Patients with SLE had higher CXCL-10 (0.164 vs 0.046ug/ml, p=0.0003) and urine CXCL-10 levels (0 vs 0 ug, p=0.01) as compared to HC. Patients with active non-renal disease had higher serum CXCL-10 levels as compared to inactive lupus (0.365 vs 0.086 pg/ml, 0.02), however, urine CXCL-10 was not significantly different between active renal and inactive subgroup. There was no difference in serum or urine CXCL-10 between active renal and active non-renal disease. [Fig 1A-D]br>
Serum galectin-9 and serum CXCL-10 showed a good association with SLEDAI2K however urinary galectin-9 and CXCL-10 had no association with SLEDAI2K [Fig 1E-H]. Serum galectin-9 and CXCL-10 levels had a modest correlation (r=0.4) with SLEDAI2K, both the urinary markers did not show any association with rSLEDAI. [Fig I-J]
In a subset of patients with active renal disease, serum galectin-9 levels significantly reduced after six-months whereas urine galectin did not show a significant fall [Fig 1K]. Serum galectin-9 showed a greater AUC than CXCL-10 (0.77 vs 0.67) in differentiating active SLE from inactive disease.
Conclusion: Serum Galectin-9 and CXCL10 are good markers of lupus activity however they do not differentiate between active renal and active non-renal disease. Urinary Galectin-9 & CXCL10 do not reflect renal activity.
Correlation of serum galectin-9 with SLEDAI 2K (E), urine galectin-9 with SLEDAI 2K (F), serum CXCL_10 with SLEDAI 2K (G) and urine CXCL_10 with SLEDAI 2K (H). Correlation of urine galectin-9 and CXCL_10 with renal SLEDAI (I, J).
Follow up levels of serum and urine galectin 9 in the active renal subgroup at baseline and 6 months (K).
To cite this abstract in AMA style:
Mehta P, Singh P, Aggarwal A. Serum Galectin-9 and CXCL-10 but Not Their Urinary Levels Reflect Lupus Activity [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/serum-galectin-9-and-cxcl-10-but-not-their-urinary-levels-reflect-lupus-activity/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-galectin-9-and-cxcl-10-but-not-their-urinary-levels-reflect-lupus-activity/