Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Idiopathic inflammatory myopathies are a heterogenous group of systemic autoimmune diseases characterized by muscle weakness. Serum cytokines and chemokines could shed light on disease pathogenesis and be used as biomarkers for prognostication, monitoring disease activity, and treatment response. We aimed to identify serum cytokine profiles of patients with active disease as compared to patients in remission and healthy controls, and explored correlations of these cytokines with clinical myositis outcome measures.
Methods: This was a prospective study of 3 clinical groups: (1) myositis patients with active disease, (2) patients in remission, and (3) healthy controls. All myositis patients fulfilled the Bohan-Peter criteria for DM/PM. Active disease was defined as requiring escalation of therapy within 6-months of screening. There were 3 study visits at baseline, 3- and 6-months. Plasma concentrations (pg/l) of 51 cytokines/chemokines/MMPs were obtained by utilizing a bead-based multiplex cytokine assay (Luminex). Physician- and patient-reported clinical outcome measures, functional measures, and creatine kinase levels were obtained for all the patients at each visit. T-test and false discovery rate for baseline differences as well as LASSO and random forest models were utilized to identify markers that best discriminate patients from controls, and patients with active disease from those in remission. GeneOntology was used for pathway analysis. Spearman correlation was used to assess correlations between cytokine levels and clinical outcome measures.
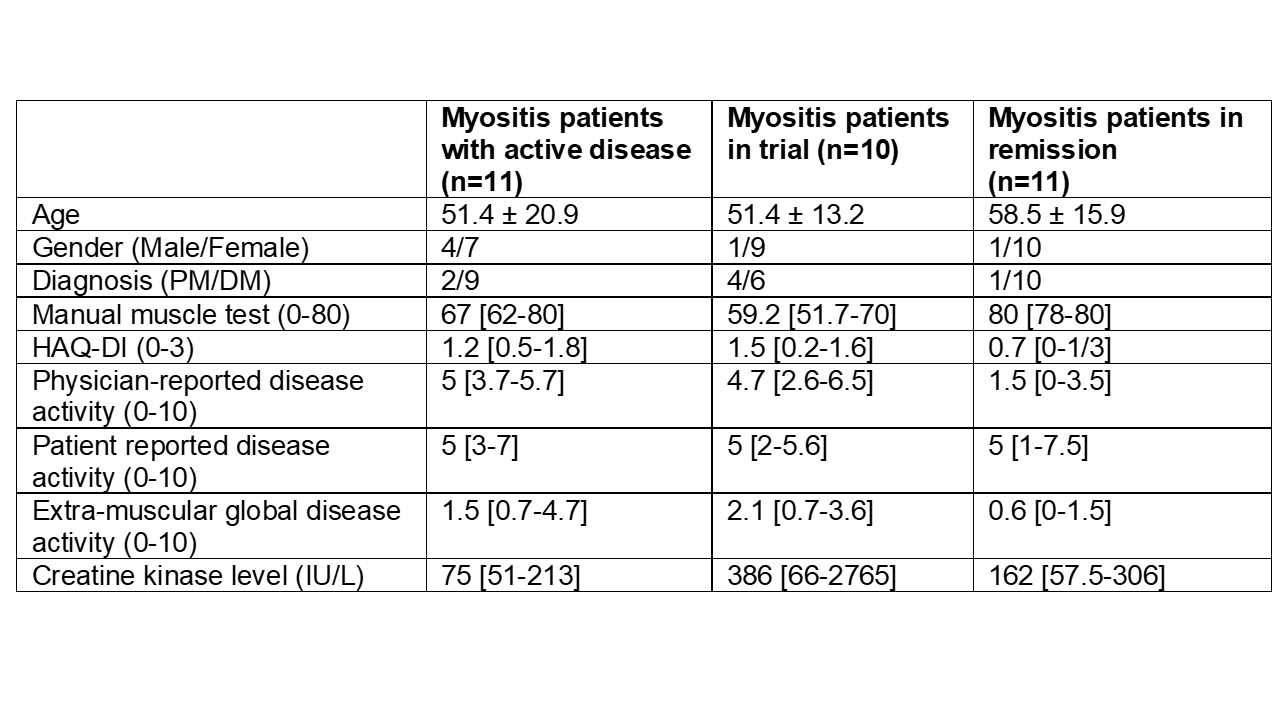
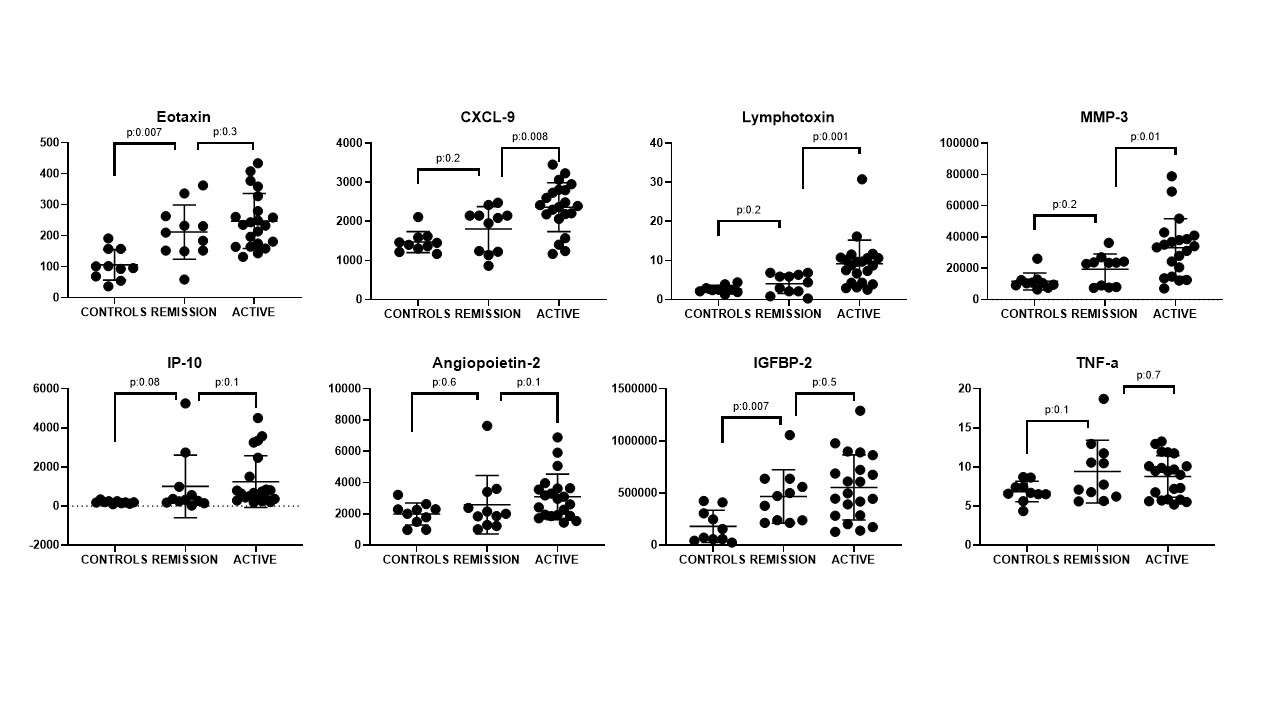
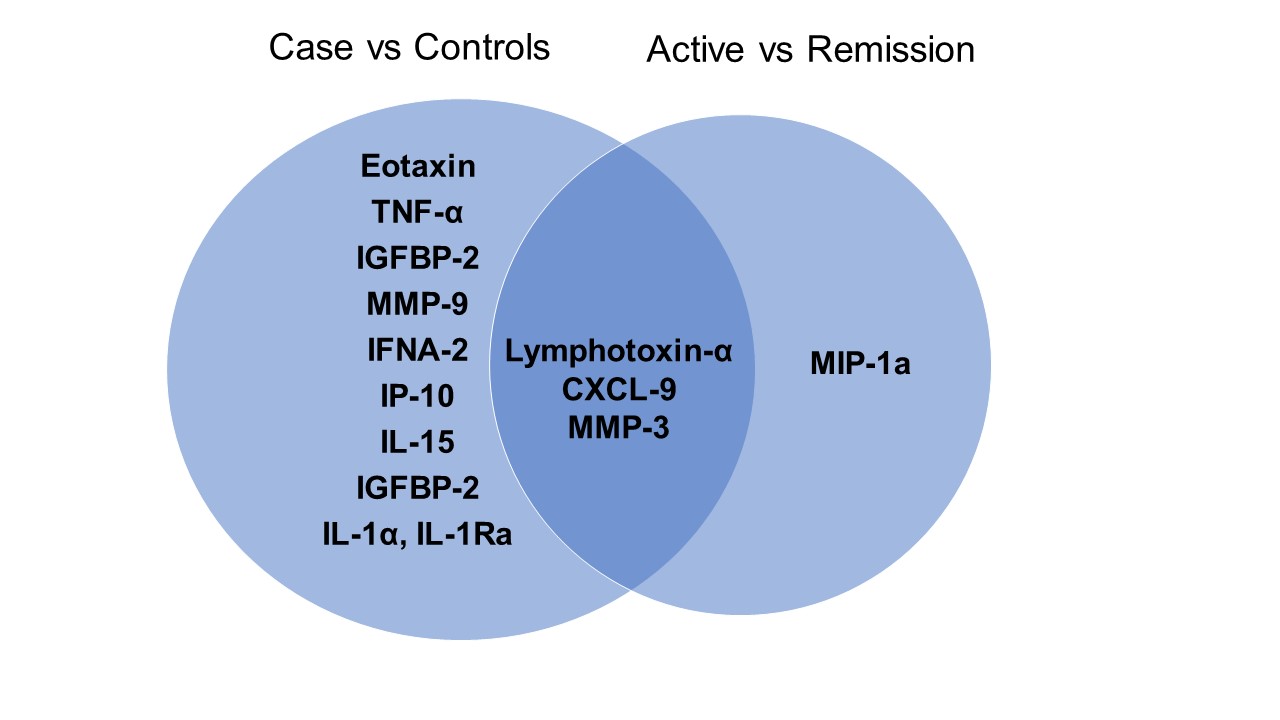
Results: 11 myositis patients in remission, 21 with active disease (including 10 enrolled in the open label trial of repository corticotropin injection) and 10 healthy controls were included in the study (Table 1). Results of the T-test, LASSO and random forest models revealed similar results. Myositis patients had elevated levels of chemokines that attract eosinophils (eotaxin) and dendritic cells, NK cells, cytotoxic T cells and monocytes/macrophages (CXCL-9, IP-10), cytokines that drive T-helper 1 responses (TNF-a, IL-1a, IL-1Ra, lymphotoxin-a, IFNA-2, IL-15), matrix degrading enzymes (MMP-3 and -9), and IGFBP-2 compared to healthy controls (Figure 1,2). Myositis patients with active disease had higher levels of lymphotoxin-a, CXCL-9, MIP-1b and MMP-3 than patients in remission. The pathways related to increased levels of these cytokines include chronic inflammatory responses, regulation of IL-1 mediated signaling, myoblast fusion, and tyrosine phosphorylation of STAT proteins. Eotaxin and CXCL-9 correlated with cutaneous and extramuscular global disease activity, IP-10 corelated with manual muscle strength test, and IL-1 correlated with HAQ as well as functional tests.
Conclusion: We identified key cytokines and chemokines that distinguish myositis patients from healthy controls as well as different disease activity states. Some cytokines correlated with clinical outcome measures, suggesting their potential use as biomarkers. Longitudinal analysis for the comparative changes in key cytokines and chemokines among different groups is currently ongoing. Larger longitudinal studies are needed to validate our findings.
To cite this abstract in AMA style:
Saygin D, Biswas P, Nouraie S, Moghadam-Kia S, McGeachy M, Oddis C, Dzanko S, Koontz D, Ascherman D, Aggarwal R. Serum Cytokine Profiles of Patients with Adult Idiopathic Inflammatory Myopathy [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/serum-cytokine-profiles-of-patients-with-adult-idiopathic-inflammatory-myopathy/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-cytokine-profiles-of-patients-with-adult-idiopathic-inflammatory-myopathy/