Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Sleep disturbances (SD) are reported to be common in RA but relatively few studies have addressed the issue. We examined the frequency and severity of self-reported poor sleep quality, symptoms of restless leg syndrome (RLS), and risk of obstructive sleep apnea (OSA) among individuals with RA, and identified predictors of SD.
Methods: Data were from FORWARD, the National Data Bank for Rheumatic Diseases, for which participants complete questionnaires every 6 months. In one questionnaire, items querying symptoms of RLS, the STOP-BANG questionnaire, a validated measure of OSA risk, physician diagnoses of OSA and RLS, and the Medical Outcomes Study Sleep Scale (MOS-S) were included. The MOS-S yields 5 subscales; results are shown here only for one (Sleep Problems Index I, SPI-I, sleep quality). was also included. Frequencies of reports of OSA risk, RLS symptoms were tabulated. Bivariate regression analyses identified predictors of OSA and RLS (logistic regression) and SPI-I scores (linear regression). Potential predictors included age, sex, race, education, smoking, Rheumatic Disease Comorbidity Index (RDCI)1, low income, obesity (BMI ≥ 30 kg/m2 and < 35), morbid obesity (BMI ≥ 35), RA duration, prednisone and other medication use, and RA disease activity (Rheumatoid Arthritis Disease Activity Index, RADAI). Variables significant in the bivariate analyses were included in multivariate regression analyses.
Results: Subject characteristics are shown in Table 1 (n = 2623). 16% reported physician-diagnosed OSA, and 14% were at high risk of OSA based on self-reported symptoms (Table 2), compared to 2-4% in the general population. Only half at high risk had an OSA diagnosis. 12% reported physician-diagnosed RLS, and 26% reported RLS symptoms, compared to ~10% in the general population. Only one third with RLS symptoms reported a physician diagnosis. Mean SPI-I was 33.4 (±18.9), ~0.5 standard deviation worse than a population sample mean. Independent predictors of high risk of OSA were male sex, obesity, current smoking, RDCI, and disease activity (Table 3). Predictors of RLS symptoms were morbid obesity and disease activity. Worse scores on SPI-I were associated with younger age, female sex, smoking, higher RDCI, shorter RA duration, and greater disease activity. OSA and RLS symptoms were also independently associated with SPI-I scores.
Conclusion: Symptoms of both OSA and RLS were more common in RA than in the population; self-reported sleep quality was also worse. Some predictors of SDs were similar to predictors in the population (e.g., age, obesity), but disease activity was also consistently associated with SD. Research in RA has linked SDs to worse outcomes. Previous research in other conditions suggests that SDs might also be a cause of increased disease activity through heighted inflammation. Further research is needed to tease out disease-specific causes and effects of SD in RA.
1 England BR et al. Arthritis Care Res 2015; 6: 865
2 Hays RD et al. Sleep Med 2005; 6:41
3 Chung F et al. J Clin Sleep Med 2014; 10:951
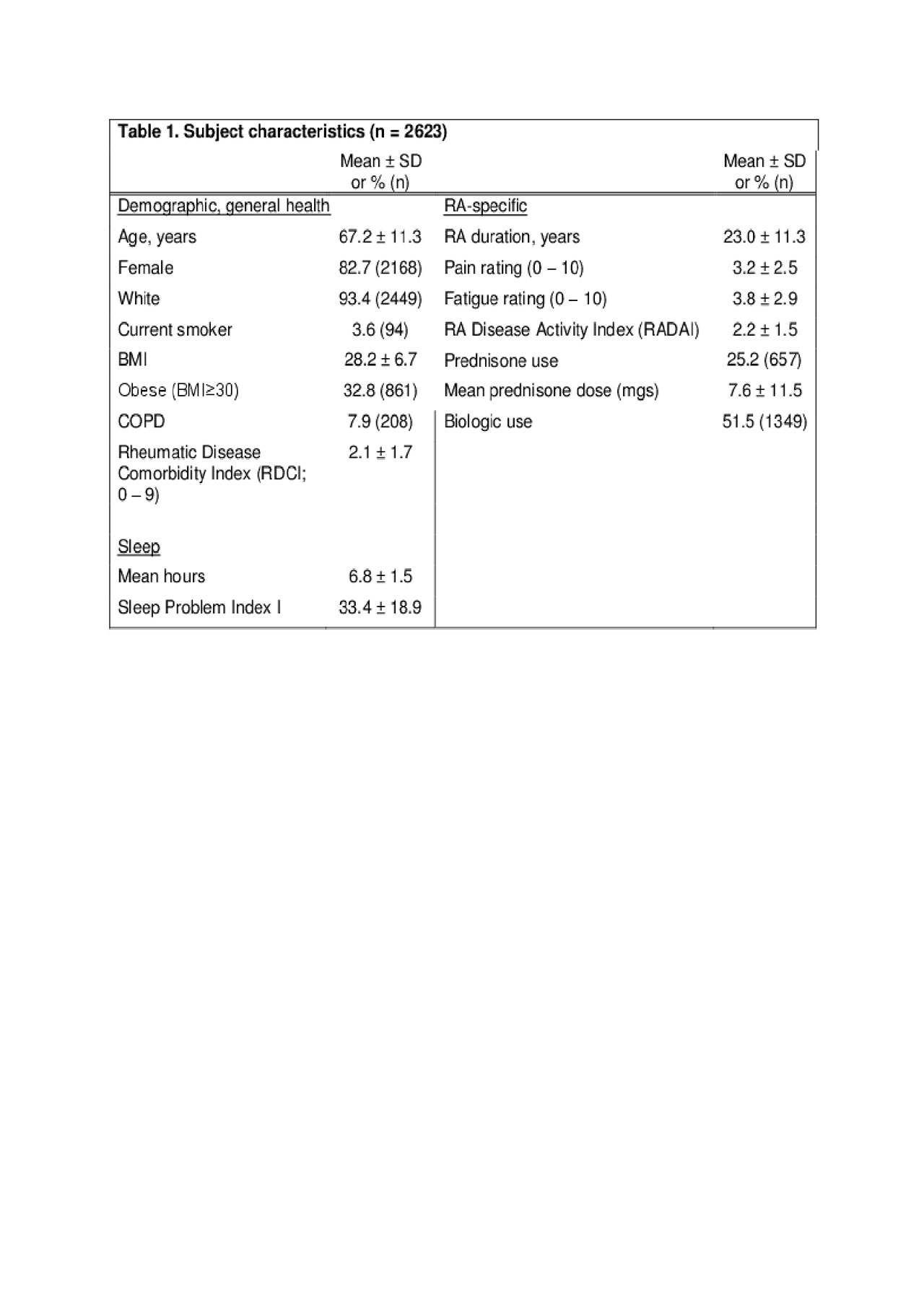
Sleep disturbances in RA table 1
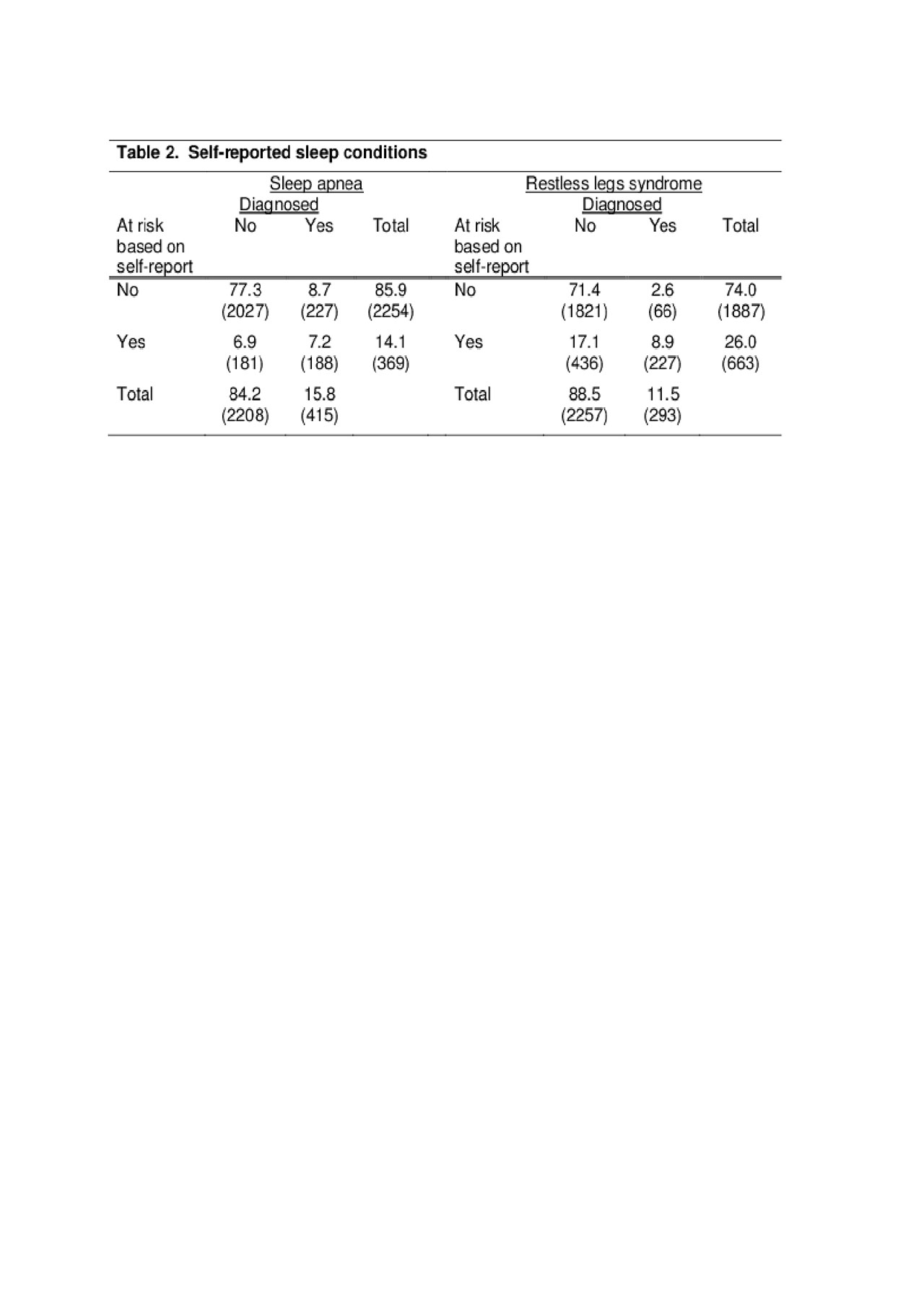
Sleep disturbances in RA table 2

Sleep disturbances in RA table 3
To cite this abstract in AMA style:
Katz P, Pedro S, Michaud K. Self-Reported Sleep Disturbances in Rheumatoid Arthritis (RA) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/self-reported-sleep-disturbances-in-rheumatoid-arthritis-ra/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-reported-sleep-disturbances-in-rheumatoid-arthritis-ra/
