Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Oral manifestations, especially periodontitis and tooth loss, are highly prevalent in patients with rheumatic diseases. Sjogren’s syndrome (SS), rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE) can present oral manifestations such as xerostomia, periodontal diseases, and oral aphthous ulcers respectively. We aimed to evaluate self-perception of oral health and habits in patients with SS, RA, and SLE.
Methods: We performed a descriptive, cross-sectional study including adult patients, who attended an academic rheumatology clinic between December 2021 and February 2024, and had a clinical diagnosis of SS, RA, or SLE. We excluded patients with dental prostheses. We applied the Geriatric/General Oral Health Assessment Index Spanish Version (GOHAI-SP) survey, which includes 12 questions on a Likert-type scale. The patients were classified based on the total GOHAI-SP score; those with ≤50 points were considered to have poor oral health, scores between 51 and 56 were considered moderate oral health, and scores ≥57 were classified as good oral health. We used descriptive statistics to report frequencies and percentages, mean (SD) or median (IQR) as appropriate. Overall scores and categories of self-perceived oral health were compared by diagnosis. A p-value < 0.05 was considered statistically significant.
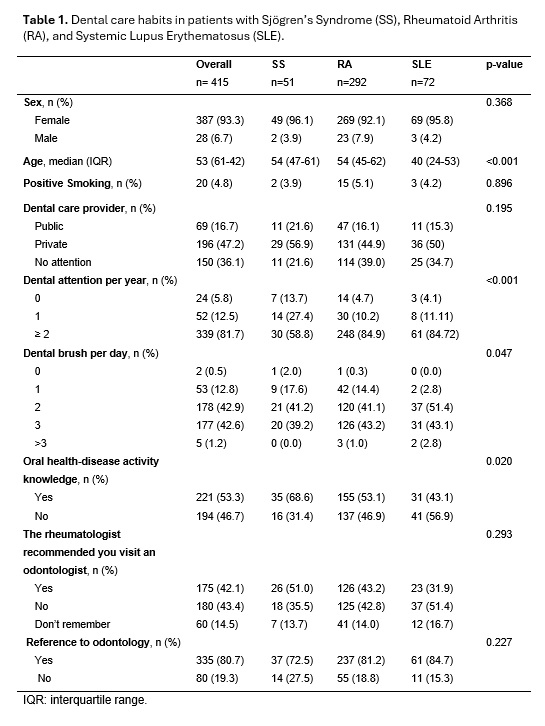
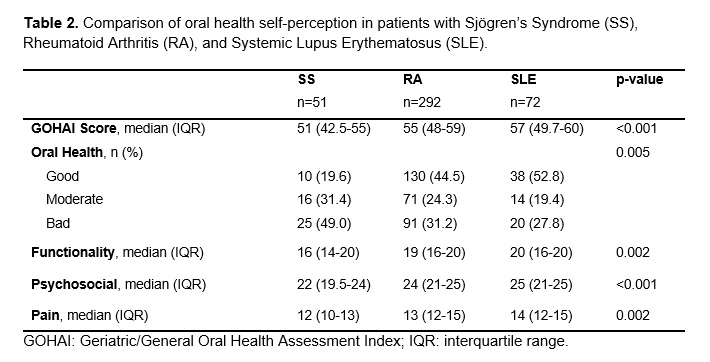
Results: We included 415 patients, with a mean age of 50.42 (SD 14.77), and 387 (93.2%) were female. Two-hundred and ninety-two patients had RA (70.8%), 72 had SLE (17.4%), and 51 had SS (11.6%). Overall, 136 patients (33%) reported poor self-perceived oral health, 101 (24.5%) moderate, and 178 (43.2%) good. The lowest median score was reported by patients with SS, 51 (42.5-55) points. Patients with SS reported a lower frequency of dental care appointments per year (< 2/year, 41.2%) and lower brush frequencies per day (£2/day, 60.8%) than patients with RA or SLE (Table 1). The patients with SS are the most aware of the relationship between their disease and oral health (68.6%) in contrast to patients with SLE (43.1%) or RA (53.1%) who are less aware (Table 1). The self-perception of oral health in the domains of functionality, psychosocial, and pain/discomfort was worse in the patients with SS (Table 2).
Conclusion: Patients with SS have poor dental habits and self-perception of functionality, psychosocial, and pain/discomfort in oral health. Patients should be advised to improve their dental habits, particularly those with SS.
To cite this abstract in AMA style:
Palomo-Arnaud K, Figueroa-Parra G, Garza-Elizondo A, Alarcon Jarquin M, Cardenas-de la Garza J, Galarza-Delgado D, Riega Torres J. Self-Perception of Oral Health and Habits in Patients with Sjögren’s Syndrome, Rheumatoid Arthritis, and Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/self-perception-of-oral-health-and-habits-in-patients-with-sjogrens-syndrome-rheumatoid-arthritis-and-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-perception-of-oral-health-and-habits-in-patients-with-sjogrens-syndrome-rheumatoid-arthritis-and-systemic-lupus-erythematosus/