Background/Purpose: Disability threatens personal independence and is a major driver of health care costs. Physical activity has been shown to prevent disability. Sedentary behavior, already associated with poor health outcomes, may have a unique relationship to the development of disability or simply reflect limited recommended moderate/vigorous physical activity (MVPA). If a separate and distinct risk factor, reducing sedentary behavior may provide an additional strategy to reduce disability among older adults.
Methods: Prospective multi-site cohort of 1680 community dwelling adults aged 49 years or older were at elevated risk to develop disability due to knee osteoarthritis or having knee osteoarthritis risk factors. Baseline sedentary and non-sedentary (e.g., light, moderate, vigorous) time were objectively measured using accelerometers. Participants were classified into sedentary time quartiles groups. Disability was ascertained from limitations in instrumental and basic activity of daily living (IADL/ADL) at baseline and two years. Hazard ratios for disability onset over 2 years follow-up were estimated from discrete time proportional hazards model controlling MVPA time, socioeconomic factors (age, sex, race/ethnicity, education, income), health factors (function, comorbidity, Center for Epidemiological Studies Depression score, body mass index category, current smoking, knee pain, knee OA severity, knee symptoms, knee injury, other lower extremity joint pain, gait speed).
Results: Incident disability was 147 versus 69, 62, and 72 per 1000 person-years over 2-years follow-up in the most sedentary quartile group (>11.5 sedentary hours per day) compared to the three less sedentary quartile groups, irrespectively. Less sedentary time was significantly associated with decreased risk of incident disability independent of moderate/vigorous minutes and other covariates (hazard ratios comparing three less sedentary quartiles vs. the most sedentary quartile, 0.62, 0.52, 0.57, irrespectively) (Figure). The average of the three less sedentary quartiles compared to the most sedentary quartile was associated with 44% decreased risk of disability (HR=0.56 [95% CI, 0.37-0.81], P=0.003). From further analyses using an isotemporal model, replacing one hour sedentary time with one hour light activity (e.g. walking) was associated with 51% decreased risk of disability onset for those in the most sedentary quartile group, independent of potential confounders and time spent in other activities (HR=0.49 [95% CI, 0.29-0.85], P=0.01; not shown in Figure).
Conclusion: Sedentary time appears to be a separate and distinct risk factor for incident disability among adults at elevated risk for disability. In addition to increasing MVPA physical activity, these findings suggest decreasing sedentary time may be an additional strategy to prevent disability onset.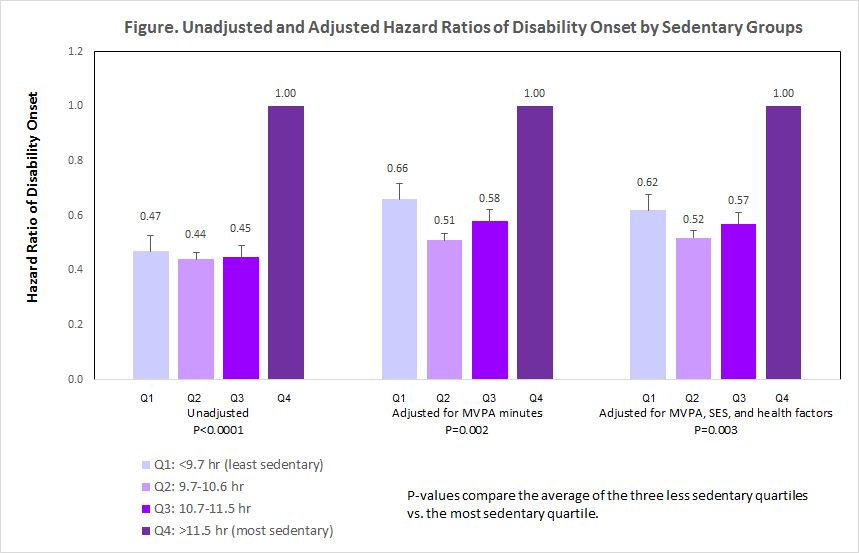
Disclosure:
J. Lee,
None;
J. Song,
None;
B. Ainsworth,
None;
R. W. Chang,
None;
L. S. Ehrlich-Jones,
None;
C. Pellegrini,
None;
P. Semanik,
None;
D. D. Dunlop,
None;
L. Sharma,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sedentary-time-is-an-independent-risk-factor-for-disability-onset-among-adults-at-elevated-risk-prospective-cohort-study/
