Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Scleroderma renal crisis (SRC) is a life-threatening vascular manifestation of systemic sclerosis (SSc) occurring in up to 5% of SSc patients. This condition continues to have significant morbidity and mortality despite the advent of angiotensin converting enzyme (ACE) inhibitors. We identified risk factors associated with SRC in addition to evaluating its management and outcomes in consecutively diagnosed patients in a large Australian tertiary referral hospital [St Vincent’s Hospital Melbourne (SVHM)].
Methods: 17 incident SRC cases were diagnosed at SVHM between 2012-2022. Patient demographics, SSc disease manifestations, and SRC treatments were determined using data prospectively collected in the Australian Scleroderma Cohort Study supplemented by chart review. Differences between those with SRC (n=17) and those without SRC (n=466) were assessed using logistic regression analyses to determine the risk factors associated with SRC.
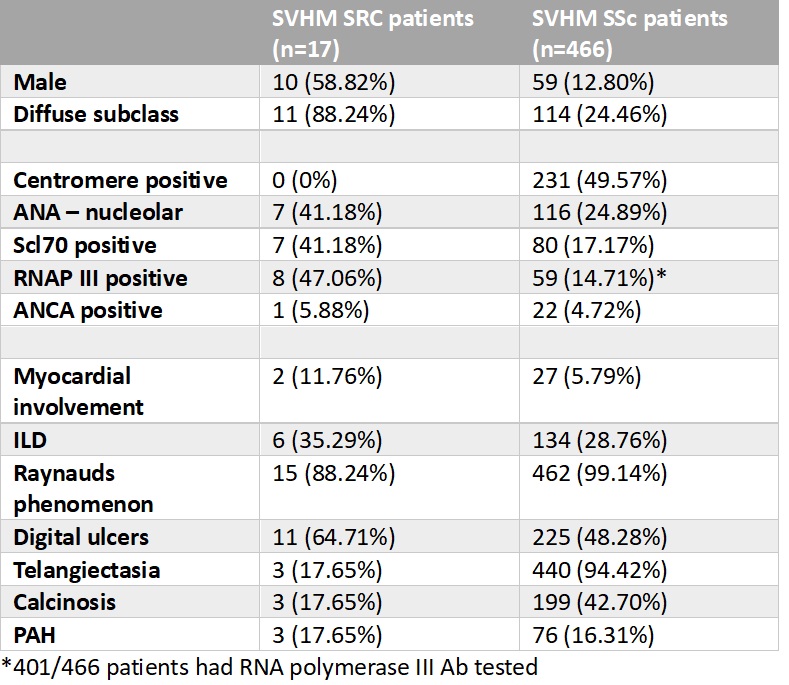
Results: There were 483 SSc patients included in this study, their demographics and disease characteristics are presented in Table 1. 17 (3.5%) of the cohort experienced SRC during our 10 year study period.
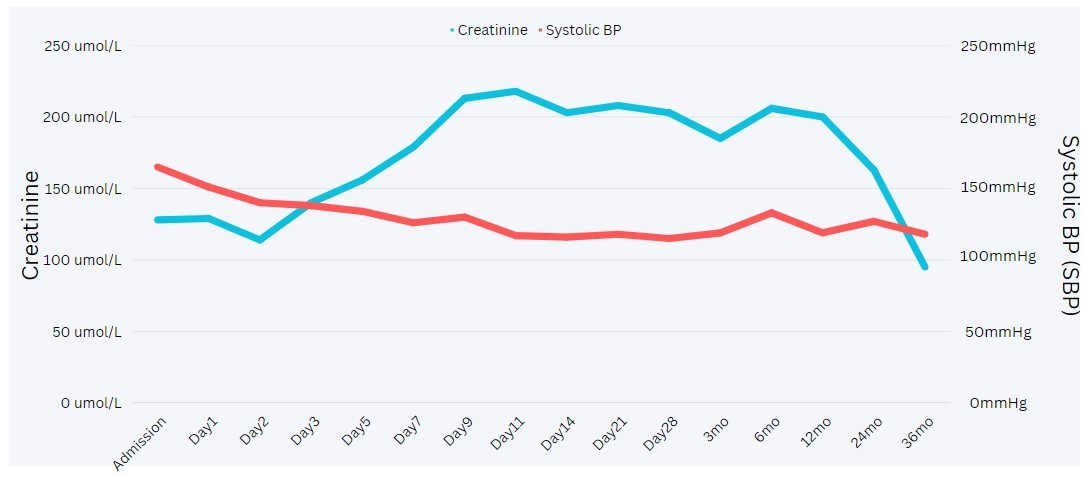
The median SSc disease duration at SRC onset was 2.5 (IQR 1-4) years. At SRC presentation, 16 patients (94.12%) presented with a systolic blood pressure (SBP) >140mmHg (median SBP = 169 (IQR 153-182)mmHg) and a median creatinine of 120 (IQR 80-156) µmol/L. Peak creatinine occurred at a median of 11 (IQR 5-14) days post SRC diagnosis, with SBP peaking at onset of SRC. Nine (52.94%) SRC patients had evidence of acute neurologic and cardiac complications including retinopathy (n=2), encephalopathy (n=6), and acute cardiac failure (n=3).
In terms of SRC management, all patients received ACE inhibitors, with a median of 3 anti-hypertensive agents required to manage hypertension. Adjuvant anti-hypertensive agents used included calcium channel blockers (most commonly amlodipine), moxonidine, and prazosin.
Complications of SRC included acute hemofiltration required in 3 (17.65%) patients, while 3 (17.65%) patients (including 2 patients that needed acute hemofiltration) required ongoing renal replacement therapy. During our observation period, 7 (41.18%) SRC patients died at a median of 2.75 (IQR 0.74-7.25) years after SRC onset, with at least 2 deaths attributable directly to complications of SRC.
Patients with SRC were more likely to be male (OR 9.73, 95% CI 3.57-26.56), have diffuse disease (OR 23.16, 95% CI 5.22-102.80), and have antibodies to Scl70 (OR 3.34, 95% CI 1.24-9.04) or RNA polymerase III (RNAP III) (OR 5.15, 95% CI 1.91-13.89).
Conclusion: In our case series, peak serum creatinine was most likely to occur 11 days after peak SBP. Refractory hypertension was a near universal feature, with adequate SBP control often requiring multiple anti hypertensives and often taking more than 7 days to achieve.
Over half of the cases of SRC in our series were negative for RNAP III, highlighting the importance of remaining vigilant for SRC, particularly in patients with diffuse disease subtype and Scl-70 antibodies.
The frequency of patients requiring renal replacement therapy (18%) in our cohort is lower than 25-81% reported in other Western countries.
To cite this abstract in AMA style:
Shah R, ross l, Morrisroe K, Stevens W, Nikpour M. Scleroderma Renal Crisis: A Large Single-center Experience [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/scleroderma-renal-crisis-a-large-single-center-experience/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/scleroderma-renal-crisis-a-large-single-center-experience/