Session Information
Date: Tuesday, November 9, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III (1836–1861)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Given the well-known burden of rheumatic disease in Canadian Indigenous populations, the Canadian Rheumatology Association (CRA) has highlighted Aboriginal Rheumatology as an area needing greater understanding, specifically on issues such as delays in care and access to specialists. Indigenous patients with rheumatoid arthritis (RA) often have worse disease than the general population yet are less likely to see specialized care. Indigenous populations appear to have earlier onset systemic sclerosis (SSc) than the general population. However, it is unclear if they experience delayed diagnosis (symptom onset to disease diagnosis), or more/less healthcare utilization during this time. We analyzed data from the Canadian Scleroderma Research Group (CSRG) registry to compare the length of time from symptom onset to disease diagnosis and healthcare utilization between North American Indigenous (NAI) and non-NAI populations. We also determined if these data were impacted by a person’s rural or urban location.
Methods: Data was obtained from the CSRG, a national longitudinal registry of patients >18 years old with SSc. All patients were included irrespective of underlying comorbidities. Patients who self-identified as Métis, Inuit and First Nations were included as NAI. We characterized the study population at entry into the registry (sex, tobacco use, income, education, location comorbidities). Location was deemed urban or rural by Canada Post guidelines. Time from first symptom to SSc diagnosis was compared between those who were and were non-NAI. Healthcare utilization related to SSc presentation (visits to health practitioners including family doctors and rheumatologists, tests done, and hospitalizations) was compared between groups.
Results: Of 1561 patients, 79 self-identified as NAI. Age, gender and comorbidities were similar between the two groups, with NAI having a higher proportion of tobacco use and lower level of education and income (Table 1). Only 19.6% of non-NAI populations lived rurally compared to 51.9% of NAI patients. There was no significant difference in time from Raynaud’s to diagnosis or 1st other symptom to diagnosis between NAI and non-NAI populations, regardless of location (Figure 2 and 3). There was also no difference in health care utilization, including visits to healthcare professionals, tests performed and hospitalizations.
Conclusion: This study suggests that, unlike other rheumatological conditions, SSc appears to be appropriately diagnosed without a time delay in those who are NAI compared to non-NAI patients. NAI SSc patients also access care at the same rate as non-NAI populations prior to SSc diagnosis.
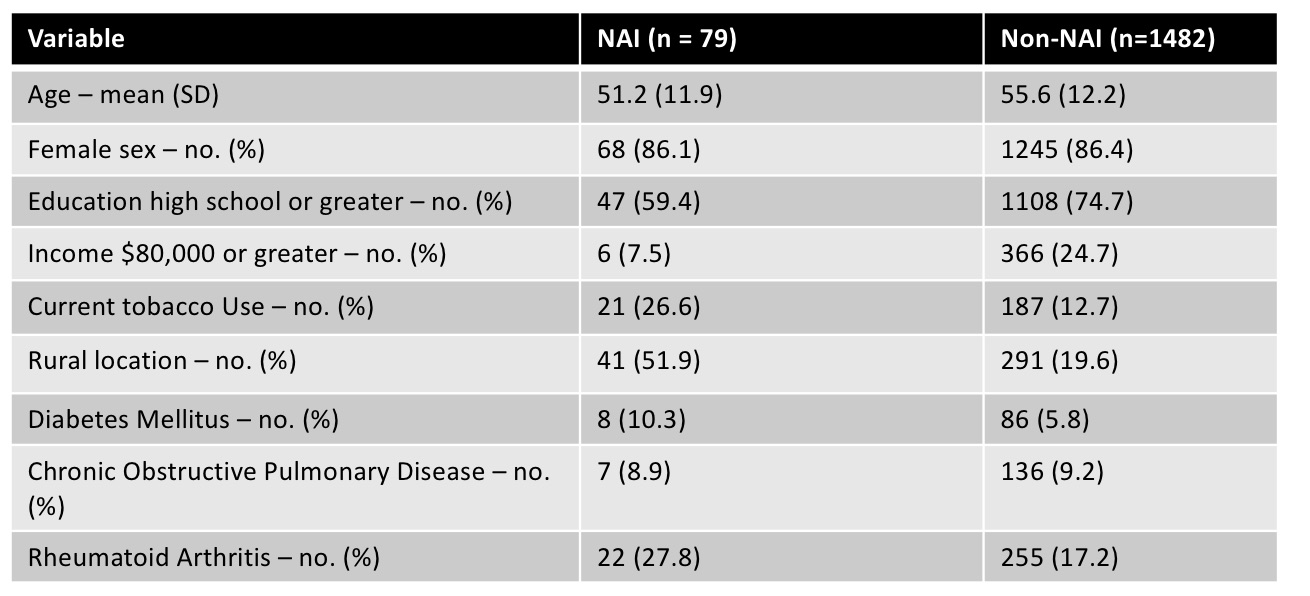 Table 1: Baseline demographics
Table 1: Baseline demographics
 Figure 2: Number of Days from Raynaud’s to systemic scleroderma diagnosis
Figure 2: Number of Days from Raynaud’s to systemic scleroderma diagnosis
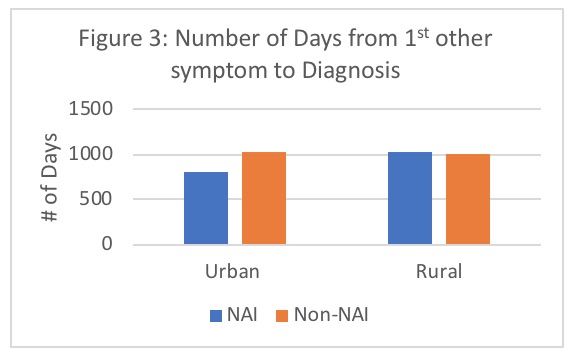 Figure 3: Number of Days from 1st other symptom to systemic scleroderma diagnosis
Figure 3: Number of Days from 1st other symptom to systemic scleroderma diagnosis
To cite this abstract in AMA style:
Sobchak C, Beattie K, Larche M. Scleroderma Presentation in the Canadian Scleroderma Research Group Indigenous Population [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/scleroderma-presentation-in-the-canadian-scleroderma-research-group-indigenous-population/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/scleroderma-presentation-in-the-canadian-scleroderma-research-group-indigenous-population/
