Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Better understanding of the abnormal immune responses in lupus nephritis (LN) is fundamental to identifying new therapies. We previously reported that the adaptor protein SAP (SLAM Associated Protein) is increased in circulating T follicular helper (TFH) and T peripheral helper (TPH) cells of patients with SLE. SAP regulates T cell function by binding to the co-stimulatory SLAMF (signaling lymphocytic activation molecule family) receptors. SAP and SLAMF are critical for TFH and TPH-dependent B cell maturation into autoantibody-producing plasma cells that characterize SLE pathogenesis. In this work, we set out to evaluate the association between circulating SAPhi T cells and clinical disease activity.
Methods: Peripheral blood mononuclear cells (PBMCs) were isolated using density gradient separation from whole blood. Cells were stained for cell surface markers, followed by permeabilization and staining of intracellular SAP. TFH were defined as CD3+CD4+CD8–PD1hiCXCR5+ and TPH were defined as CD3+CD4+CD8–PD1hiCXCR5–. Other markers included CXCR3, CCR4, CCR6, CD25, CD127 and HLADR. Additionally, we analyzed SAP expression from renal infiltrating LN T cells using the publicly available single-cell RNA sequencing (sc-RNA Seq) Accelerated Medicines Partnership (AMP) in SLE dataset. (Nat Immunol 2019; 20: 902-914.)
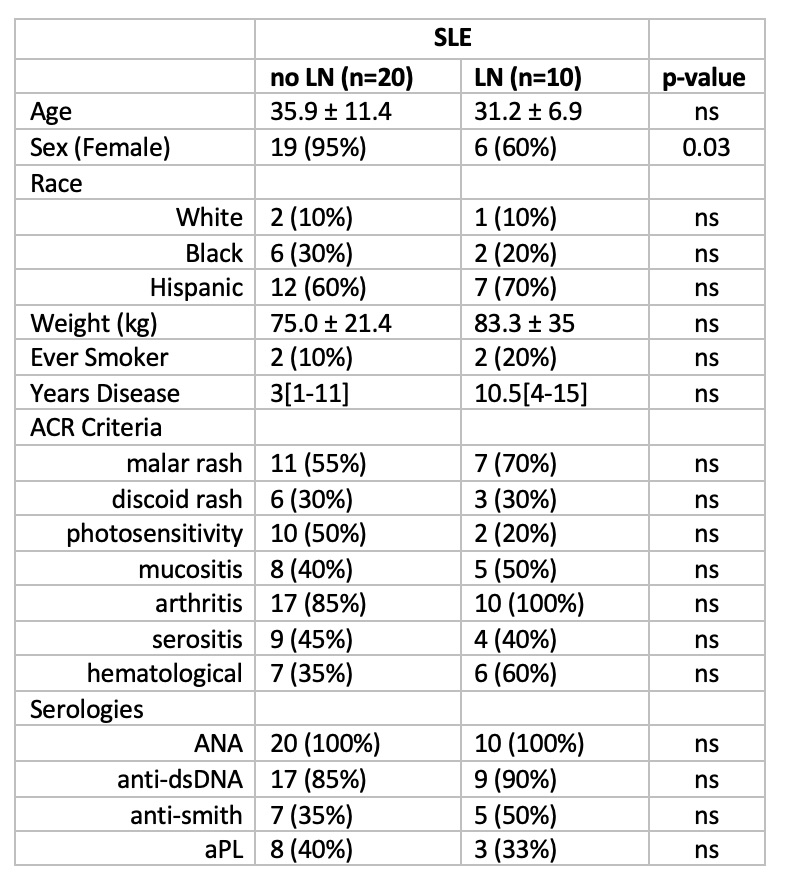
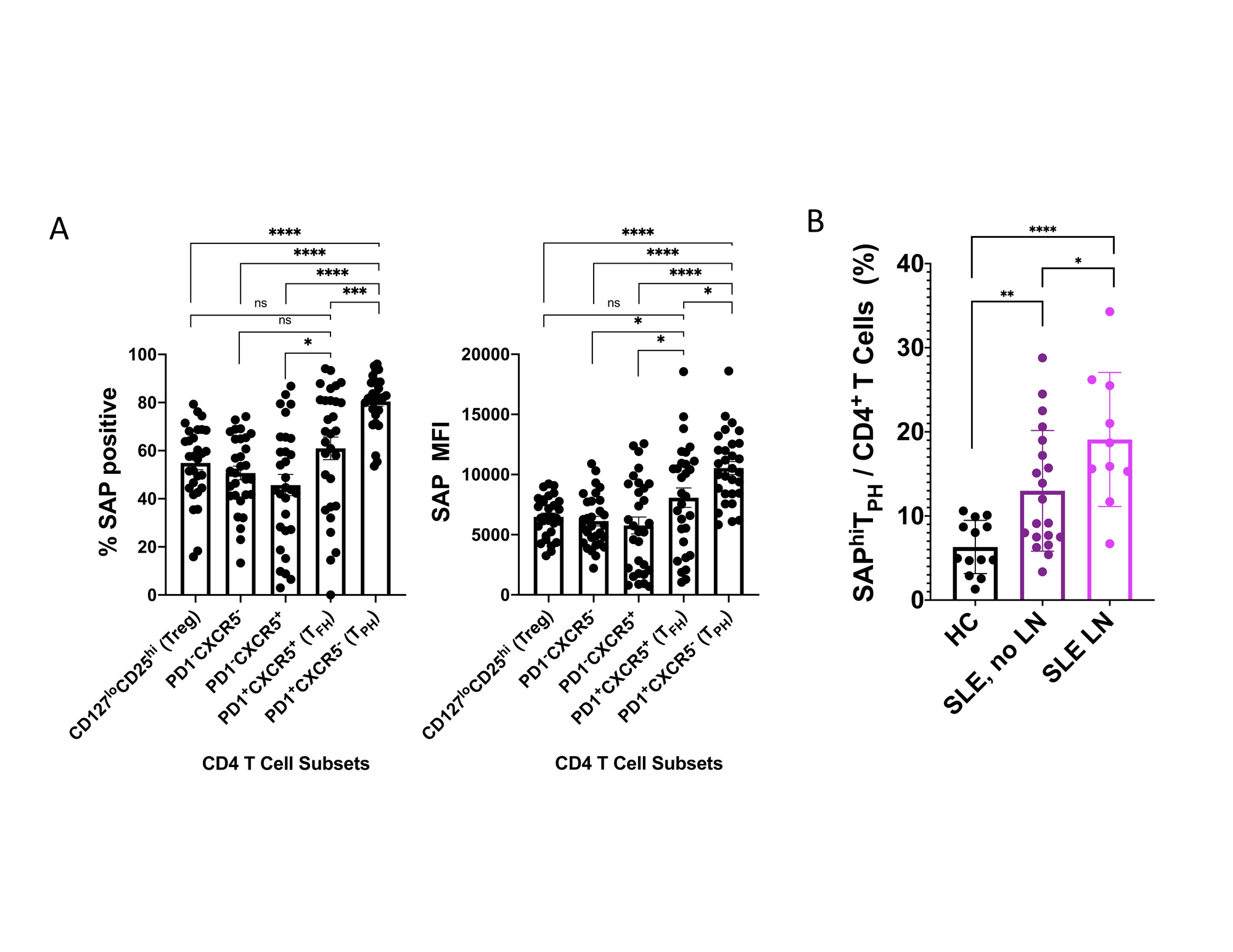
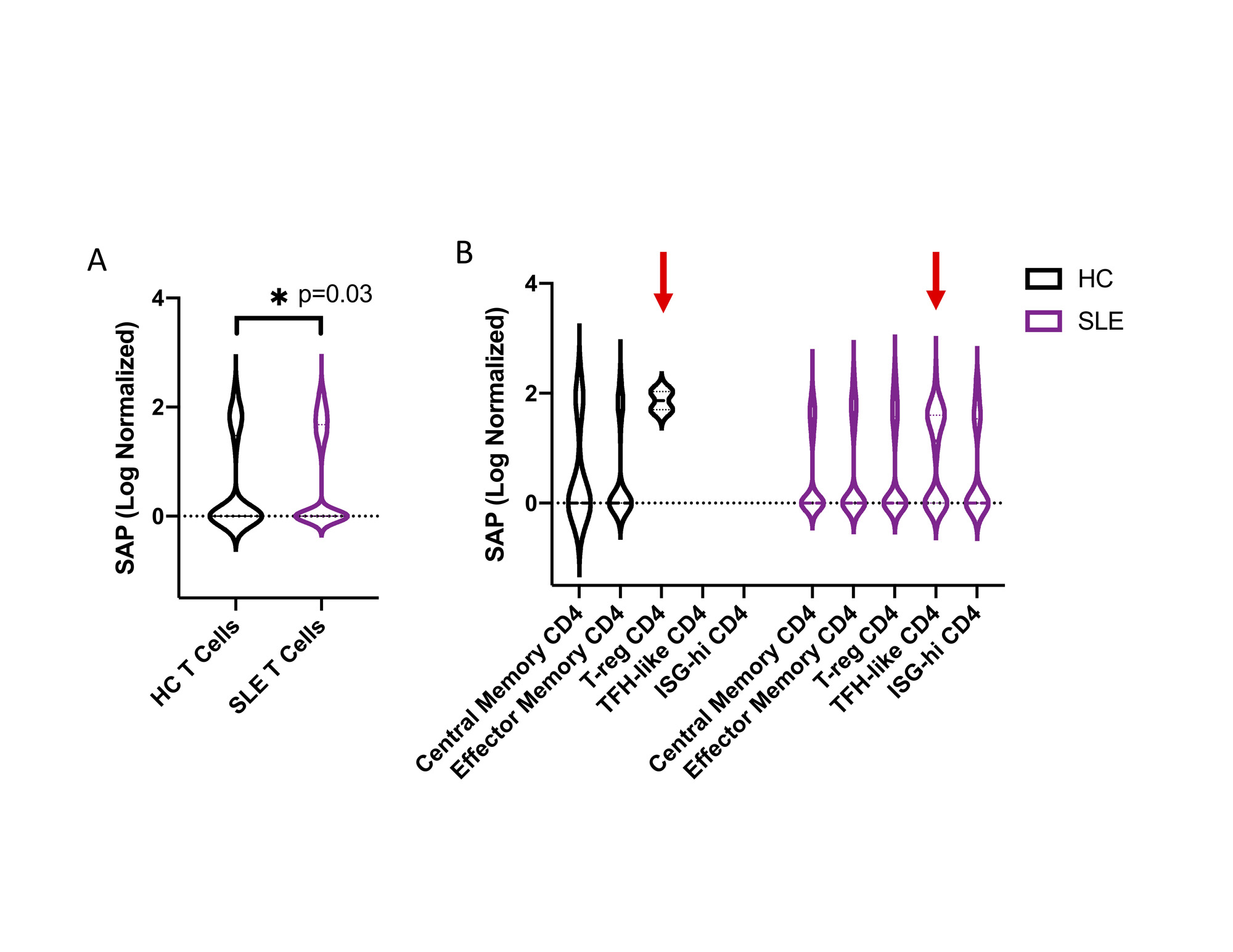
Results: PBMCs from 35 patients with SLE (1997 ACR criteria), including 10 patients with LN, were analyzed. The clinical characteristics are presented in Table 1. Mean age was 34±10, 83% were female. Males were more likely to have LN (p=0.03). We found an increase in total SAP-positive CD4 and CD8 T cells in SLE compared with controls (56±16 vs. 41±12 and 53±16 vs 39±10, respectively). In CD4 T cells, the highest SAP expression was in the TPH, detectable in > 90% of TPH cells in some patients. (Fig. 1A) The percent of SAPhiTPH in circulation was associated with SLEDAI-2K (Pearson r=0.5, p=0.01) and showed a trend for inverse association with C3 and C4 levels. SAPhiTPH cells were expanded in SLE patients presenting with flare vs. no flare. A sub-analysis revealed an association with active urine sediment, elevated anti-dsDNA, and nephrotic syndrome. SLE patients with renal disease had higher levels of circulating SAPhiTPH, and the association between SAPhiTPH and LN remained significant after adjusting for age, sex, race, low complements, and elevated anti-dsDNA (p=0.02).(Fig. 1B)To validate these findings we used the AMP scRNA-Seq data. Using the authors’ clustering analysis, we found a small but statistically significant increase in SAP levels from renal infiltrating T cells from SLE compared with control kidney biopsy samples (p=0.03). Notably, SAP expression in CD4 T cells was differentially upregulated in the TFH-like vs. the T-regulatory subsets in the SLE vs. control group. (Fig. 2)
Conclusion: We identified that SAPhiTPH cells are associated with active SLE, specifically LN. Furthermore, we validated the presence of an analogous SAPhi TFH-like subset in the LN kidney biopsy samples, suggesting direct tissue-level infiltration by these cells. Future work to improve our understanding of SAP functions and signaling in these cells is likely to reveal novel therapeutic targets in SLE.
To cite this abstract in AMA style:
Gartshteyn Y, Khalili L, Geraldino-Pardilla L, Mor A, Askanase A. SAPhigh T Peripheral Helper Cells Are a Novel Subset Associated with Lupus Nephritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/saphigh-t-peripheral-helper-cells-are-a-novel-subset-associated-with-lupus-nephritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/saphigh-t-peripheral-helper-cells-are-a-novel-subset-associated-with-lupus-nephritis/