Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: We aimed to assess whether there is a rural-urban disparity in the incidence of myocardial infarction (MI) hospitalization in patients with rheumatoid arthritis (RA).
Methods: We used the 2016-2019 U.S. data that provides a nationally representative data on all hospitalizations in the U.S. Rural/urban residential status was identified using the NIS PL_NCHS variable, with micropolitan or not metropolitan or micropolitan counties being defined as rural. We assessed the multivariable adjusted odds ratios (aOR) to examine the association of rural residence with MI hospitalization with urban residence as the reference category, while adjusting for demographics, payer, income, hospital characteristics, and the Deyo-Charlson Comorbidity Index, a composite validated comorbidity score commonly used to account for the varying effect of 19 common comorbidities.
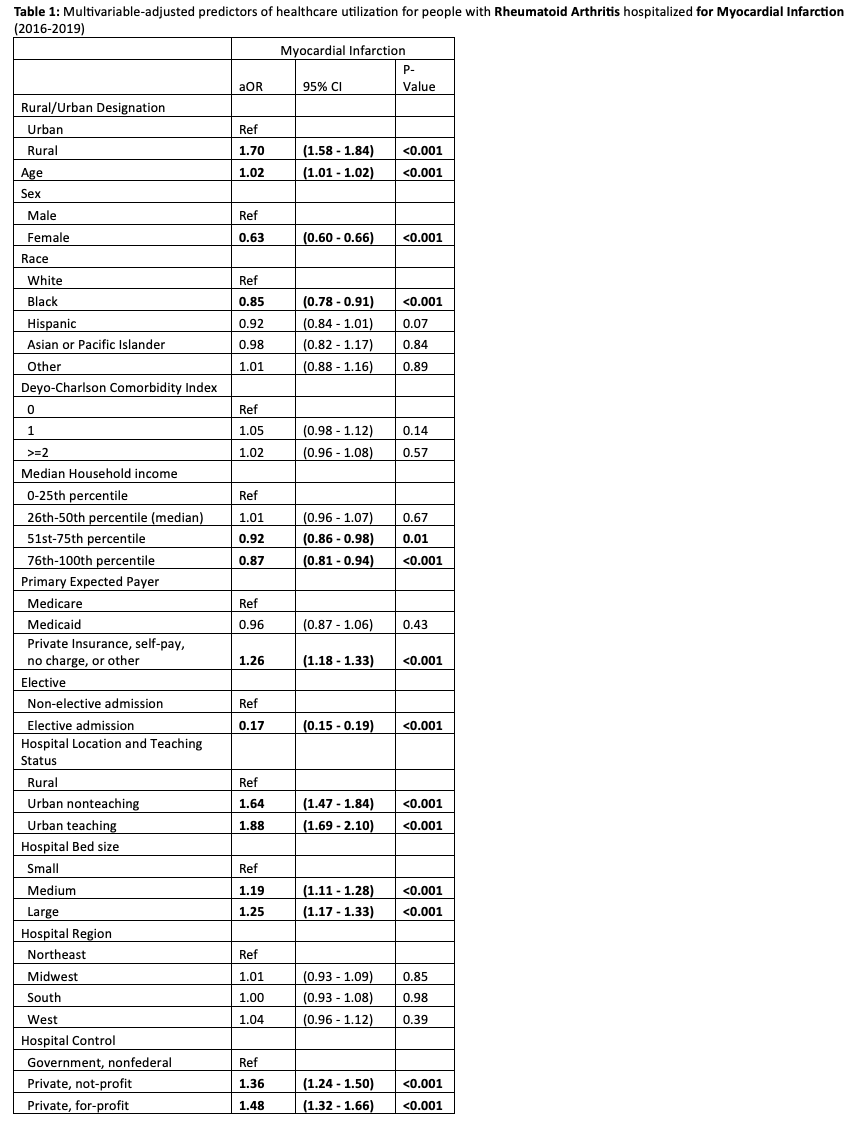
Results: The crude rate of MI hospitalization for 100,000 area specific RA hospitalizations was significantly higher for rural versus urban Residents, 2,441 versus 1,878 (p< 0.001). In multivariable adjusted models, compared to urban residence, rural-residing residents with RA had almost twice as likely to be hospitalized with MI with an adjusted odds ratio (aOR) of 1.70 (95% CI, 1.58, 1.84, p< 0.001; Table 1). Compared to lowest quartile, the two highest income quartiles were significantly and independently associated with lower odds of MI hospitalization in RA, aOR were 0.92 (95% CI, 0.86 - 0.98) and 0.85 (95% CI, 0.81 - 0.94, p< 0.001; Table 1). Female sex, African American race, elective admission, Medicare payer, government hospital control, rural hospital location, small hospital bed size, were significantly associated with a lower odds of MI hospitalization (Table 1). The adjusted higher odds of MI hospitalizations in RA patients were confirmed in several sensitivity analyses that: (1) excluded elective admission status, aOR 1.53 (1.42 - 1.65, p< 0.001); (2) Including interaction term for rurality and sex, age, and Deyo-Charlson comorbidity index aOR 1.45 (1.07 - 1.98, p=0.02); (3) consisting of individual Deyo-Charlson comorbidities rather than a categorical scale, aOR 1.53 (1.42 - 1.64, p< 0.001).
Conclusion: Our study findings of rural-urban and SES disparities for MI hospitalizations in RA provide policymakers with data and information for action, that could be used for policy decisions to reduce these gaps, to improve outcomes in rural residents that would also improve overall outcomes.
To cite this abstract in AMA style:
Chandrupatla S, Singh J. Rural-dwelling Patients with Rheumatoid Arthritis or Those with Lower Income Are More Likely to Be Admitted for Myocardial Infarction in the U.S. and Have Worse Outcomes [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/rural-dwelling-patients-with-rheumatoid-arthritis-or-those-with-lower-income-are-more-likely-to-be-admitted-for-myocardial-infarction-in-the-u-s-and-have-worse-outcomes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rural-dwelling-patients-with-rheumatoid-arthritis-or-those-with-lower-income-are-more-likely-to-be-admitted-for-myocardial-infarction-in-the-u-s-and-have-worse-outcomes/