Session Information
Date: Tuesday, November 9, 2021
Title: Abstracts: RA – Diagnosis, Manifestations, & Outcomes II: Heart & Lung (1915–1918)
Session Type: Abstract Session
Session Time: 2:00PM-2:15PM
Background/Purpose: Many guidelines recommend limiting glucocorticoids to short-term use in patients with rheumatoid arthritis (RA), but up to 40% of patients remain on glucocorticoids long-term. In this study we evaluated the cardiovascular risk of long-term, low-dose glucocorticoid use by studying patients on stable DMARD treatments.
Methods: Using Medicare claims and Optum’s deidentified Clinformatics Data Mart from 2006 to 2015, we identified patients with RA (2 diagnosis codes ≥7 days apart) who remained on stable DMARD therapy for >180 days (no gaps >90 days and no new DMARDs), excluding patients with previous myocardial infarction (MI), stroke, coronary artery bypass grafting, or percutaneous coronary intervention using all available data during or prior to the baseline period. The 180 days before DMARD initiation and the first 180 days of stable DMARD course comprised the baseline period. Average glucocorticoid dose was assessed during the final 90 days of the baseline period and categorized as none, ≤5mg, 5-10mg, or >10mg/day. Inverse probability weights for the likelihood of being prescribed each glucocorticoid dose category were constructed using multinomial logistic regression. Cause-specific proportional hazards models with inverse probability weights and clustering to account for patients with multiple treatment periods were used to estimate the effect of glucocorticoid use on composite cardiovascular outcomes (stroke or MI). Patients were censored at the end of the stable DMARD course, end of enrollment, 9/30/2015, death in Medicare data, or 90 days after a change in glucocorticoid dose category (the completion of a treatment period). Predicted 1-year incidence of events was calculated from the weighted models to estimate risk by glucocorticoid dose while controlling for confounding factors.
Results: There were 188,940 treatment periods among 135,583 patients in Medicare and 51,295 treatment periods among 39,272 patients in Optum (Table 1). Medicare patients had 158,839 years at risk with 2,067 composite cardiovascular outcomes and Optum patients had 36,876 years at risk with 313 outcomes corresponding to an incidence of 1.3 and 0.8 per 100 person-years, respectively. In Medicare, glucocorticoids were associated with a dose-dependent increase in cardiovascular risk in weighted models (Table 2) with predicted 1-year incidence of 1.4% (95% CI 1.2-1.6) for ≤5mg, 1.7% (1.4-2.0) for 5-10mg, and 1.9% (1.3-2.7) for >10mg versus 1.1% for no glucocorticoids (Figure 1). Unadjusted results were similar in the younger Optum population, but adjusted results were not significant with predicted 1-year incidence of 0.9% (95% CI 0.7-1.1), 0.8% (0.5-1.2), and 0.8% (0.4-1.8), respectively, versus 0.7% with no glucocorticoids.
Conclusion: Among older RA patients on stable DMARD therapy, long-term use of low-dose glucocorticoid was associated with increased risk for stroke or MI. Higher doses of glucocorticoids were associated with even greater risk. The absolute risk in the younger Optum cohort was lower and research with larger patient populations will be needed to determine if risks exist among younger patients with lower baseline cardiovascular risk.
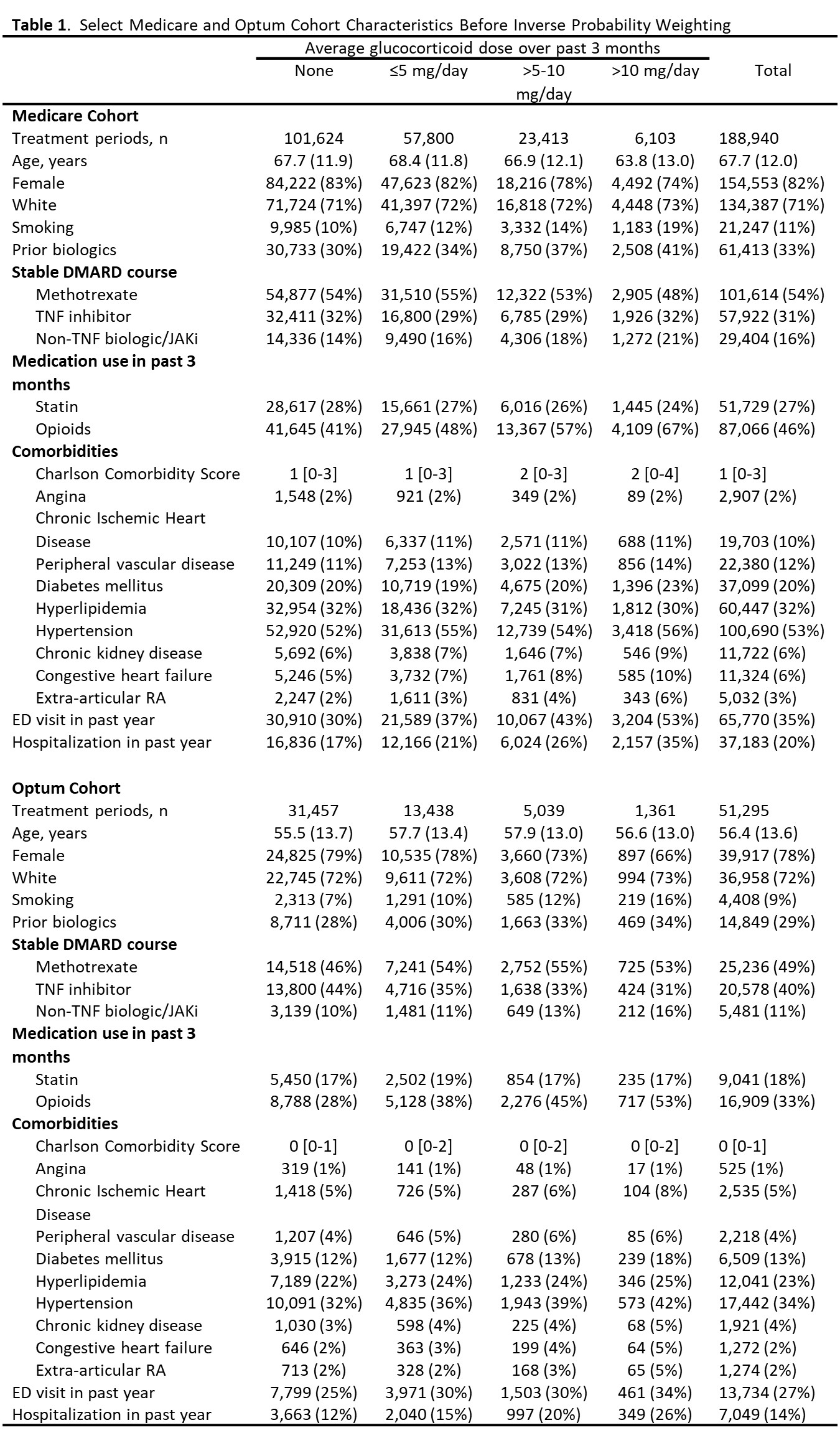 Values are in the format: mean (standard deviation), n (%), or median [interquartile-range]
Values are in the format: mean (standard deviation), n (%), or median [interquartile-range]
 Hazard ratios (HR) and confidence intervals (CI) are from unadjusted cause-specific proportional hazard models and from propensity adjusted models using stabilized inverse probability weights (IPWS). * Incidence per 100 person-years
Hazard ratios (HR) and confidence intervals (CI) are from unadjusted cause-specific proportional hazard models and from propensity adjusted models using stabilized inverse probability weights (IPWS). * Incidence per 100 person-years
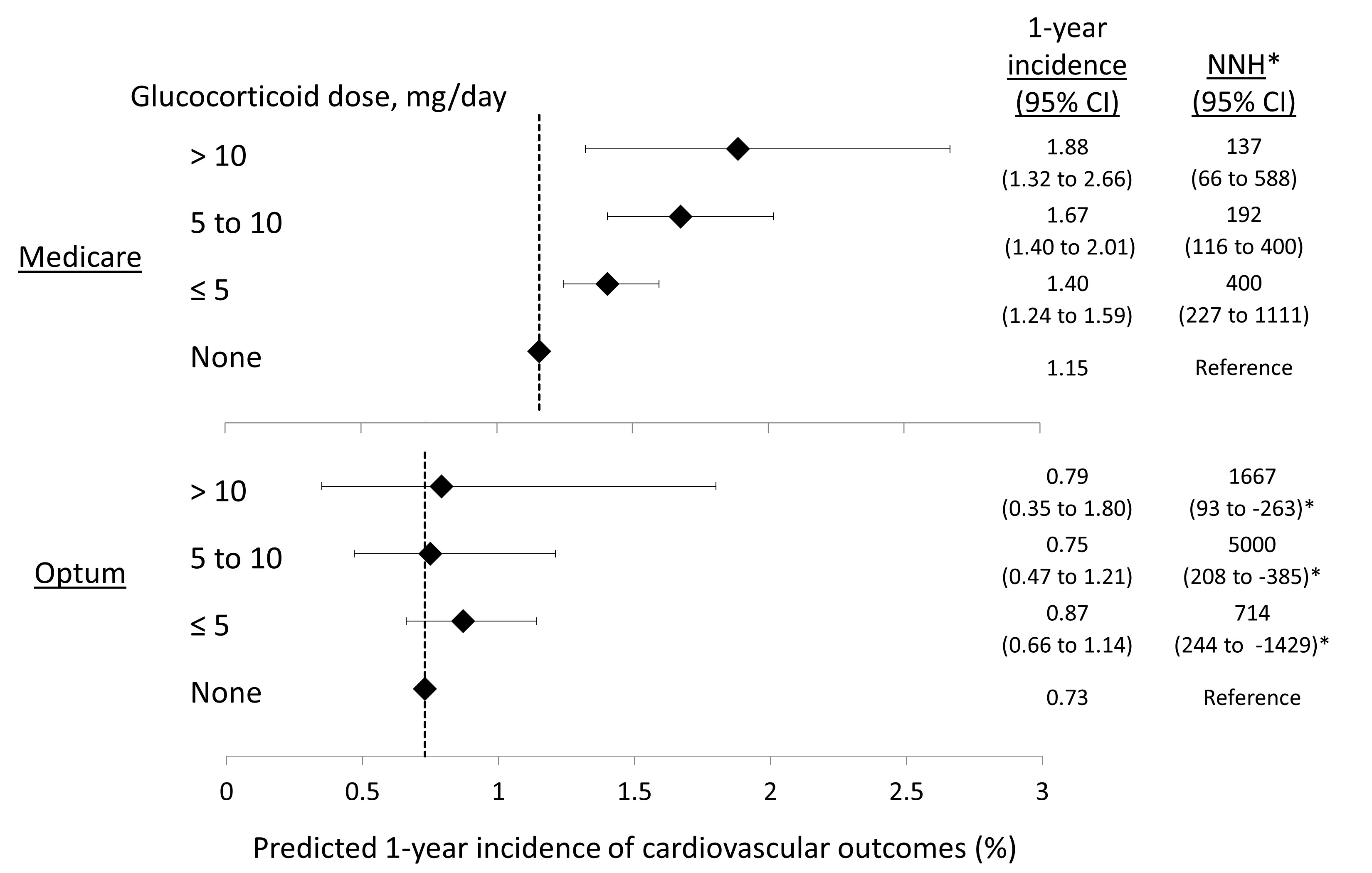 Predicted 1-year incidence of myocardial infarction or stroke calculated from inverse probability weighted cause-specific hazards models. Hazard ratios for these models are shown in Table 2. * NNH = number needed to harm. The NNH 95% confidence intervals (CI) for each glucocorticoid dose category in the Optum dataset overlaps with the reference estimate for no glucocorticoids. Negative estimates can be interpreted as the number needed to treat to avoid a composite cardiovascular outcome.
Predicted 1-year incidence of myocardial infarction or stroke calculated from inverse probability weighted cause-specific hazards models. Hazard ratios for these models are shown in Table 2. * NNH = number needed to harm. The NNH 95% confidence intervals (CI) for each glucocorticoid dose category in the Optum dataset overlaps with the reference estimate for no glucocorticoids. Negative estimates can be interpreted as the number needed to treat to avoid a composite cardiovascular outcome.
To cite this abstract in AMA style:
Coburn B, George M, Baker J, Hsu J, Wu Q, Chen L, Xie F, Yun H, Curtis J. Risk of Cardiovascular Outcomes with Low-Dose Glucocorticoids in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/risk-of-cardiovascular-outcomes-with-low-dose-glucocorticoids-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-cardiovascular-outcomes-with-low-dose-glucocorticoids-in-patients-with-rheumatoid-arthritis/
