Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: There is evidence of an increased risk of cardiovascular disease in several autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus. In primary Sjögren’s syndrome (pSS), evidence of cardiovascular risk is limited and inconsistent. The aim of the study was to evaluate if the risk of atherosclerotic cardiovascular disease (myocardial infarction, ischaemic or haemorrhagic stroke, and peripheral artery disease), venous thromboembolism, heart failure and cardiovascular mortality is increased in patients with pSS compared to matched population comparisons.
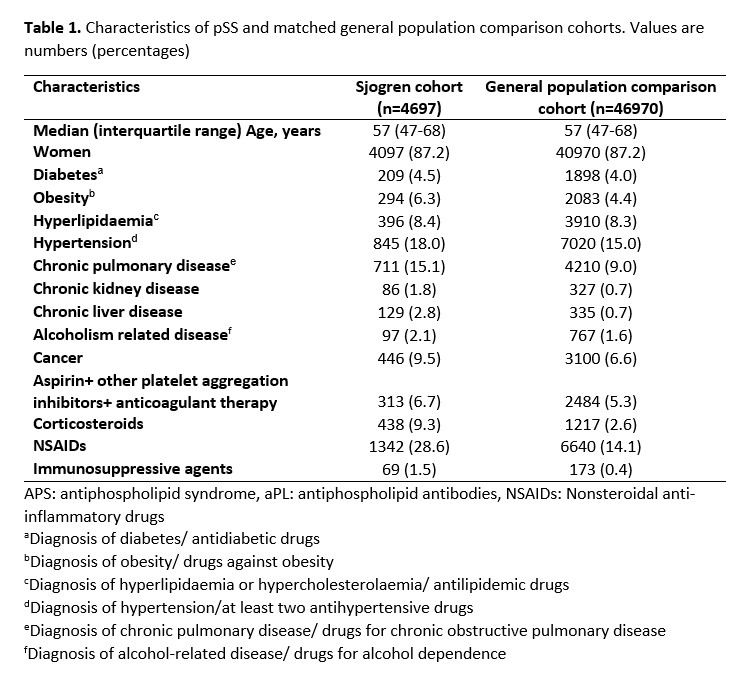
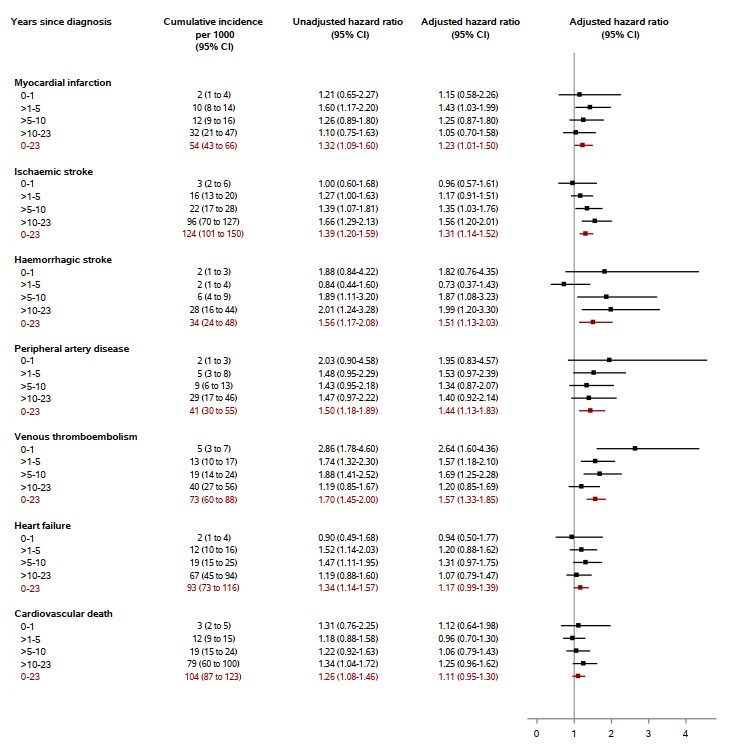
Methods: We conducted a nationwide, population-based cohort study including all patients with a pSS diagnosis from 1996 to 2017, matched with a control cohort on age, gender and calendar year. Diagnoses are coded according to the International Classification of Diseases, eighth Revision (ICD-8) through 1993 and 10th Revision (ICD-10) thereafter. All patients with autoimmune disease associated with pSS and any patient diagnosed with cardiovascular disease before the index date were excluded. For each outcome, the cumulative incidence was calculated and a Cox regression analysis was performed to calculate adjusted hazard ratios for comorbidities. Several stratifications (on age, sex, selected drugs, number of cardiovascular risk factors) and sensitivity analyses were performed.
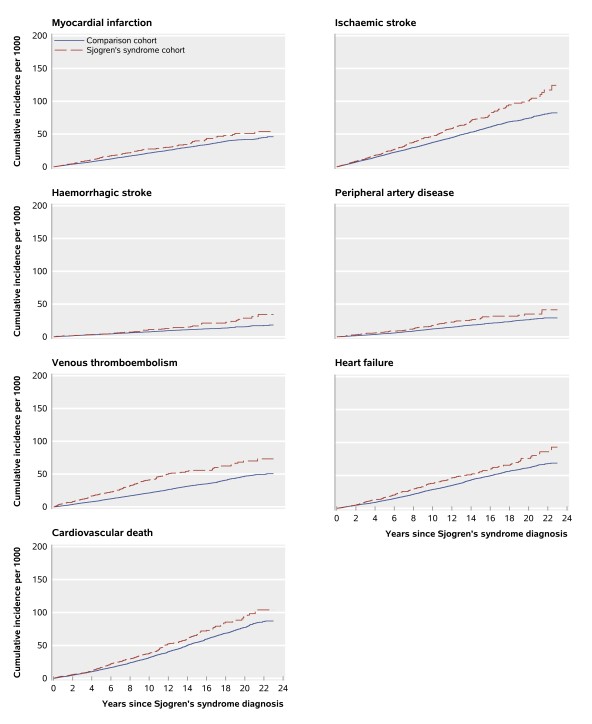
Results: In this study, 4697 pSS patients and 46970 people in the comparison cohort were included. Among patients with incident pSS (median age 57 years, women 87.2%), a higher absolute risk of most clinical outcomes was observed compared with the general population. The cumulative incidences per 1000 people for the pSS cohort compared with the general population after a maximum of 23 years of follow-up were 54 versus 46 for myocardial infarction, 93 versus 69 for heart failure, 124 versus 82 for ischaemic stroke, 34 versus 18 for haemorrhagic stroke, 41 versus 29 for peripheral artery disease, and 73 versus 51 for venous thromboembolism. Using Cox regression for confounder adjustment, pSS was clearly associated with increased rates of myocardial infarction (adjusted hazard ratio=1.23; 95% confidence interval 1.01-1.50), ischaemic and haemorrhagic stroke (1.31; 1.14-1.52 and 1.51; 1.13-2.03, respectively), peripheral artery disease (1.44; 1.13-1.83), and venous thromboembolism (1.57; 1.33-1.85). The risks of deep vein thrombosis (1.80; 1.45-2.23), pulmonary embolism (1.35; 1.06-1.72), as well as provoked (1.60; 1.26-2.03) and unprovoked (1.74; 1.40-2.17) venous thromboembolism were also increased in pSS patients. Cardiovascular mortality (1.11; 0.95-1.30) and the risk of heart failure (1.17; 0.99-1.39) was modestly yet imprecisely increased in pSS.
Conclusion: pSS was associated with clearly increased risks of venous thromboembolism and all atherosclerotic cardiovascular outcomes, and with modest risk increases for heart failure and cardiovascular death. These findings may relate to pro-thrombotic state and atherosclerosis induced by chronic inflammation in pSS and highlight the clinical importance of managing cardiovascular risk factors in patients with pSS.
To cite this abstract in AMA style:
Loiseau P, Mailhac A, Duhaut P, Toft Sørensen H, W Thomsen R. Risk of Atherosclerotic Cardiovascular Events and Venous Thromboembolism in People with Primary Sjögren’s Syndrome: A Danish Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/risk-of-atherosclerotic-cardiovascular-events-and-venous-thromboembolism-in-people-with-primary-sjogrens-syndrome-a-danish-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-atherosclerotic-cardiovascular-events-and-venous-thromboembolism-in-people-with-primary-sjogrens-syndrome-a-danish-cohort-study/