Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Utilization of total hip (THA) and total knee arthroplasty (THA) remains high for patients with RA, and most patients have moderate to high disease activity at the time of surgery. Risk of infection and transfusion are higher compared to OA, and transfusion at the time of surgery increases the risk of perioperative infection. Tranexamic acid (TXA), an anti-fibrinolytic, has gained widespread use in total joint arthroplasty to decrease transfusions, but benefits in RA has not been established. We aimed to determine the risk factors for transfusion for patients with RA undergoing THA/TKA, and assess the use of TXA in decreasing transfusions.
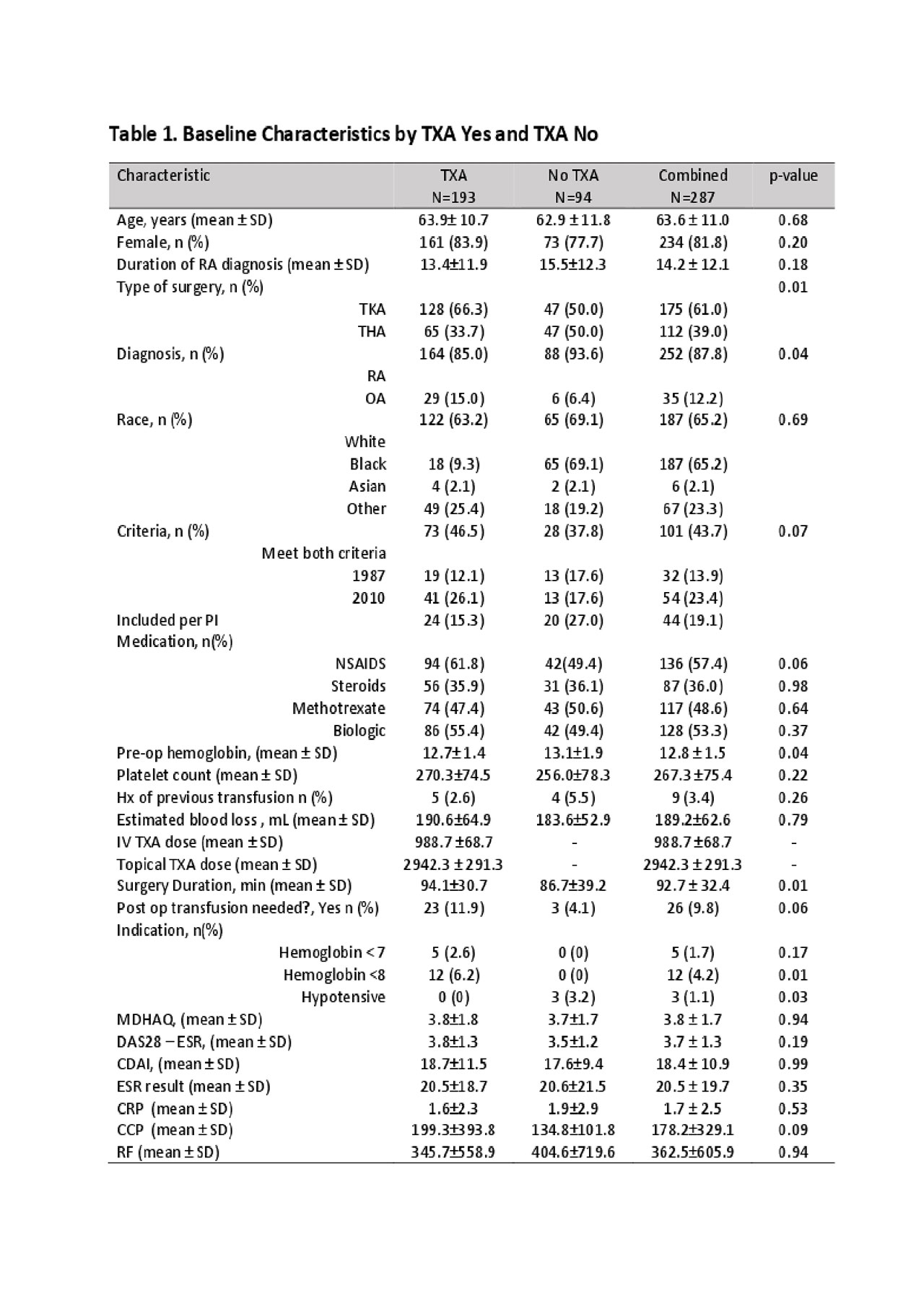
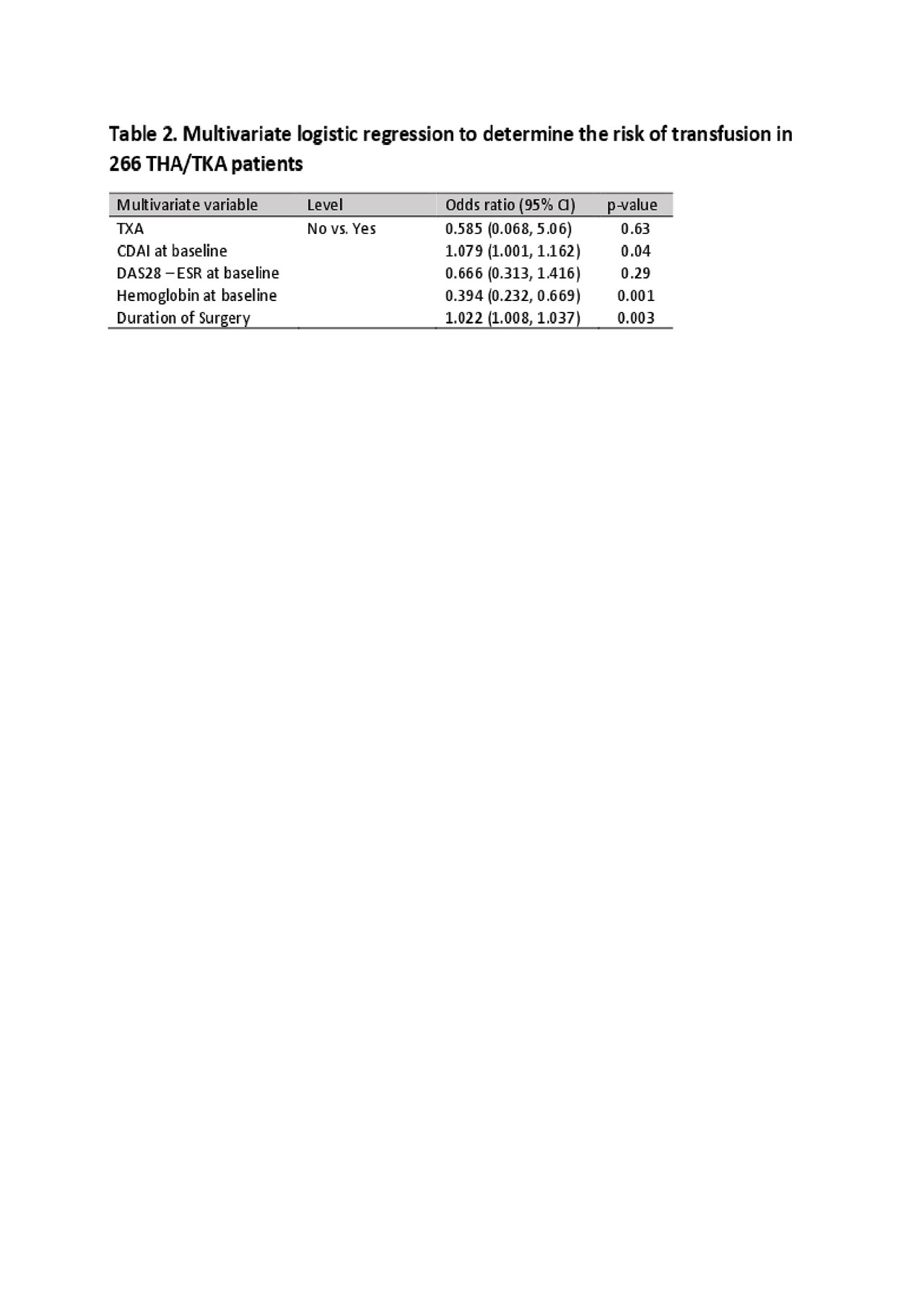
Methods: We retrospectively reviewed data from a prospectively collected cohort of 233 patients with RA and a convenience sample of 35 OA controls undergoing THA/TKA. Demographics, RA characteristics, and disease activity were systematically collected and hemoglobin and TXA use obtained by chart review. Disease activity was measured utilizing the DAS28 and CDAI, PROMs included HOOS/KOOS, and MDHAQ, and ESR, and CRP, and serologies were drawn pre-op. Baseline characteristics were summarized using descriptive statistics and compared using Chi-squared, Fisher’s exact test or two-sample t-test or Wilcoxon rank-sum test as appropriate. Logistic Regression analysis was performed to explore the relationship between transfusion (Yes or No) and predictors (including CDAI, DAS28, TXA received or not). Predictors that were found statistically significant (p< 0.05) in the univariate analysis were included in the multivariate analysis.
Results: RA cases were predominantly women (83%), with prolonged disease duration(14.1 +/-12 years), and active disease (mean DAS28= 3.7, CDAI=18.4±10.9), (TABLE 1). Transfusions were received by 26 RA(11.2%). TXA was given in 193 patients (67.3%, OA 83% vs RA 67%).There was no difference in blood loss or transfusion for those undergoing TKA vs THA (p=.32). Patients who received TXA required more transfusions than those who did not (11.9% vs. 4.1%, p >0.05). In the univariate analysis, baseline hemoglobin, estimated blood loss, duration of surgery, baseline CDAI and baseline ESR increased the risk of transfusion. In the multivariate analysis to determine independent risk factors for transfusion (Table 2), a one g/dl decrease in baseline hemoglobin (OR=0.394, 95% CI (0.232, 0.669), p=0.001) , one-minute increase in surgical duration (OR=1.022, 95% CI (1.008, 1.037), p=0.003) and a one-point increase in CDAI (OR=1.079, 95% CI (1.001, 1.162) were significant. TXA was not associated with post-operative transfusion in either the univariate or multivariate analysis.
Conclusion: Pre-surgical optimization should include assessment and treatment of anemia in patients with RA who undergo total joint arthroplasty. This is important, as TXA was not associated with a lower transfusion rate as reported for patients with OA. Decreased pre-operative hemoglobin may be a modifiable risk factor, while increased disease activity as measured by CDAI and increased surgical time were risk factors for post-operative transfusion but may be more difficult to change in these patients with long standing RA.
To cite this abstract in AMA style:
Morse K, Abolade J, Heinz N, Zhang M, Russell L, Mirza S, Orange D, Wright-Chisem J, Figgie M, Sculco P, Goodman S. Risk Factors for Transfusion and Use of Tranexemic Acid in Patients with Rheumatoid Arthritis Undergoing Total Hip Arthroplasty and Total Knee Arthroplasty [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-transfusion-and-use-of-tranexemic-acid-in-patients-with-rheumatoid-arthritis-undergoing-total-hip-arthroplasty-and-total-knee-arthroplasty/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-transfusion-and-use-of-tranexemic-acid-in-patients-with-rheumatoid-arthritis-undergoing-total-hip-arthroplasty-and-total-knee-arthroplasty/