Session Information
Date: Monday, November 14, 2022
Title: Abstracts: Epidemiology and Public Health II: COVID, Infection and Pregnancy Outcomes
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Reported infection rates and severe outcomes of COVID-19 in patients with immune-mediated inflammatory diseases (IMIDs) and their therapy, have varied depending on the nature and size of the study population, and the presence or absence of control populations. Having a more reliable analysis of larger populations, with consideration of vaccination status and comorbidities is essential for current and future pandemics.
Methods: All patients (pts) testing positive by SARS-CoV-2 PCR and NAAT test were identified from 51 hospitals and 1,085 clinics in Providence St. Joseph Health, which serves seven US states. IMID pts, subsetted into those typically seen by a rheumatologist and those by other specialists were identified. Outcomes were hospitalization and death within 30 days of the first COVID infection. Two time periods were analyzed: 03/01/2020 – 12/25/2021: pre-Omicron, 12/26/2021 – 04/13/2022: Omicron. Immunomodulatory medications were observed for three months prior to the index date. Risk factors, including IMIDs, medications, demographics, comorbidities, and vaccination status were analyzed using multivariable logistic regression and gradient boosting (XGBoost).
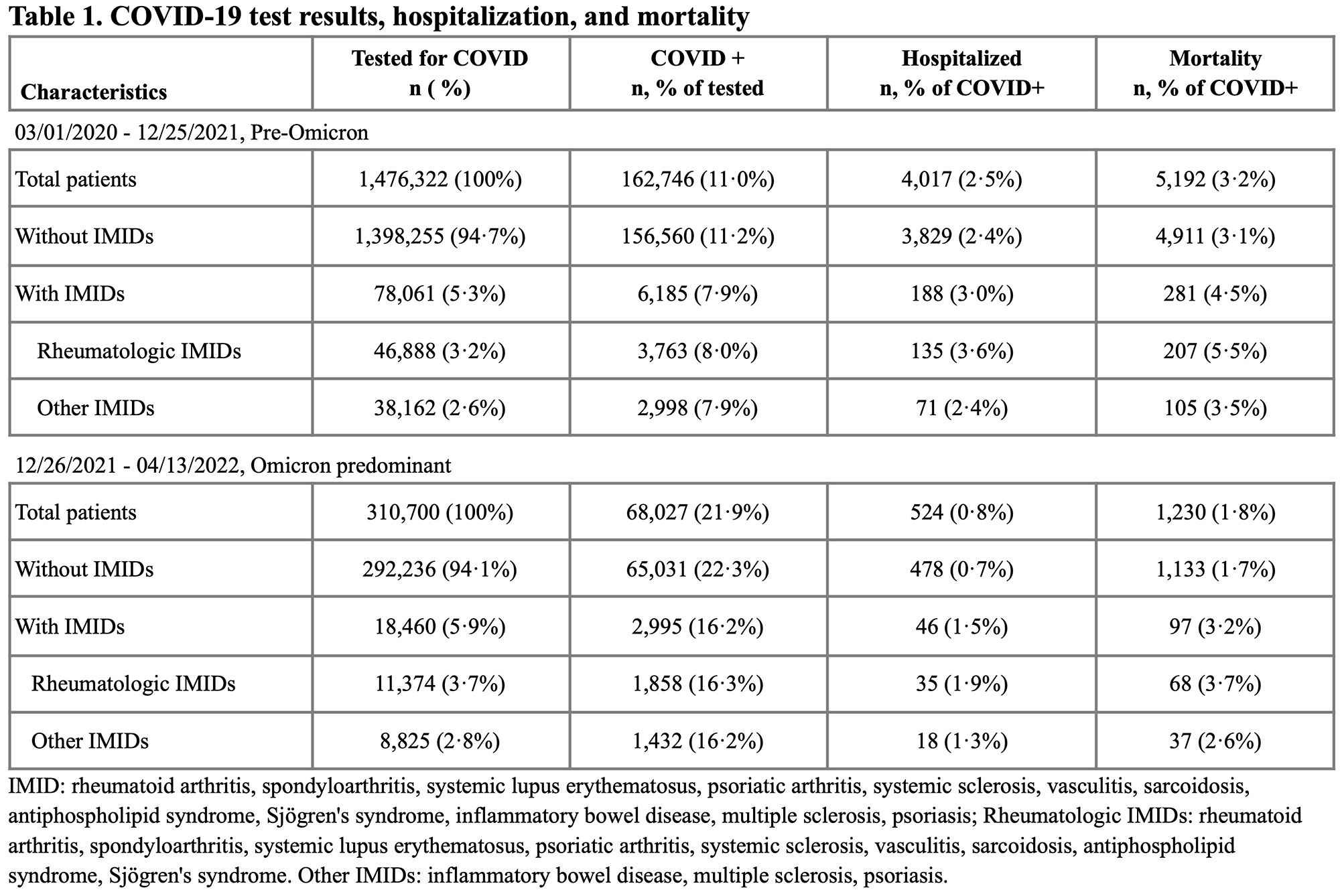
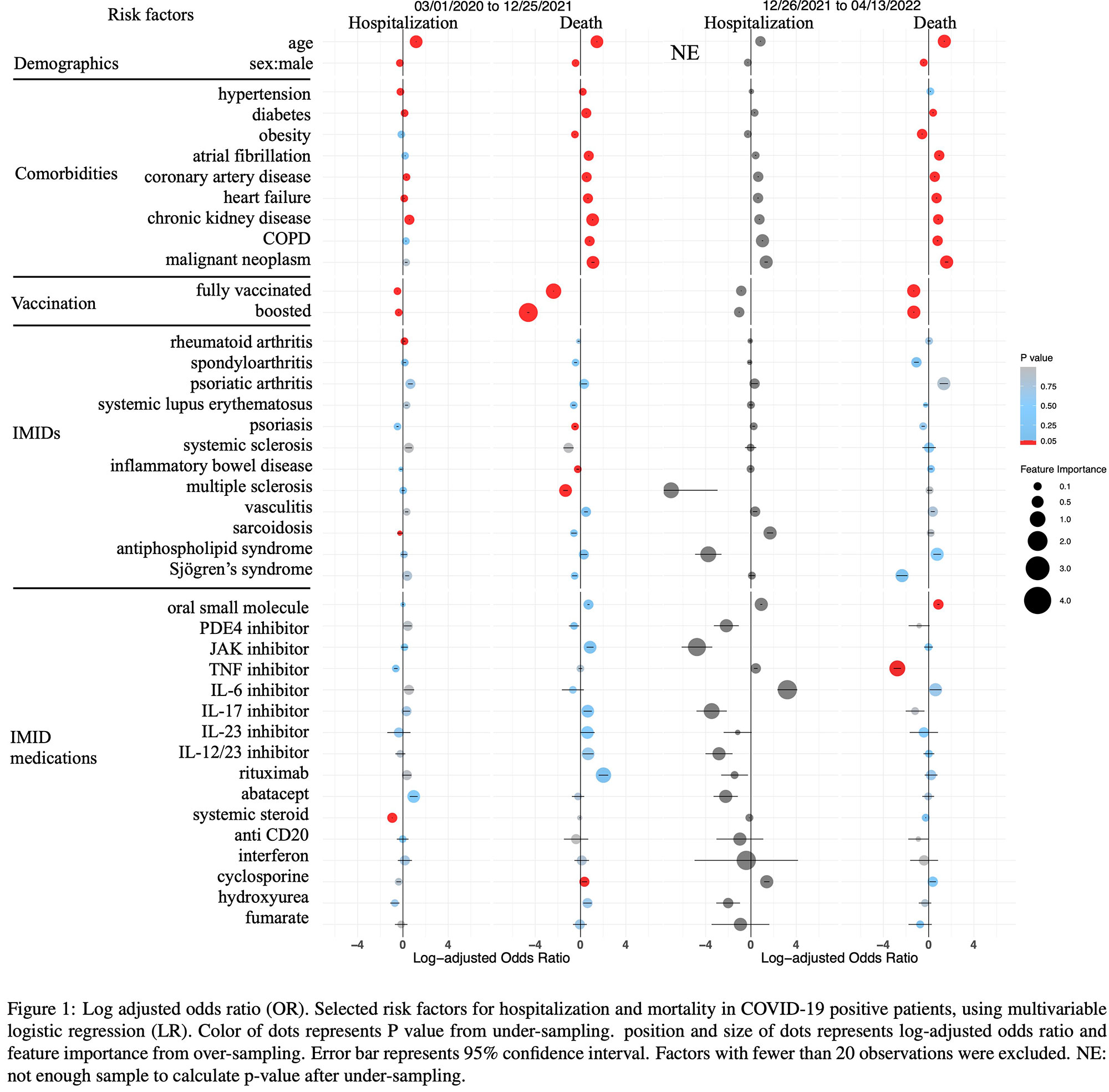
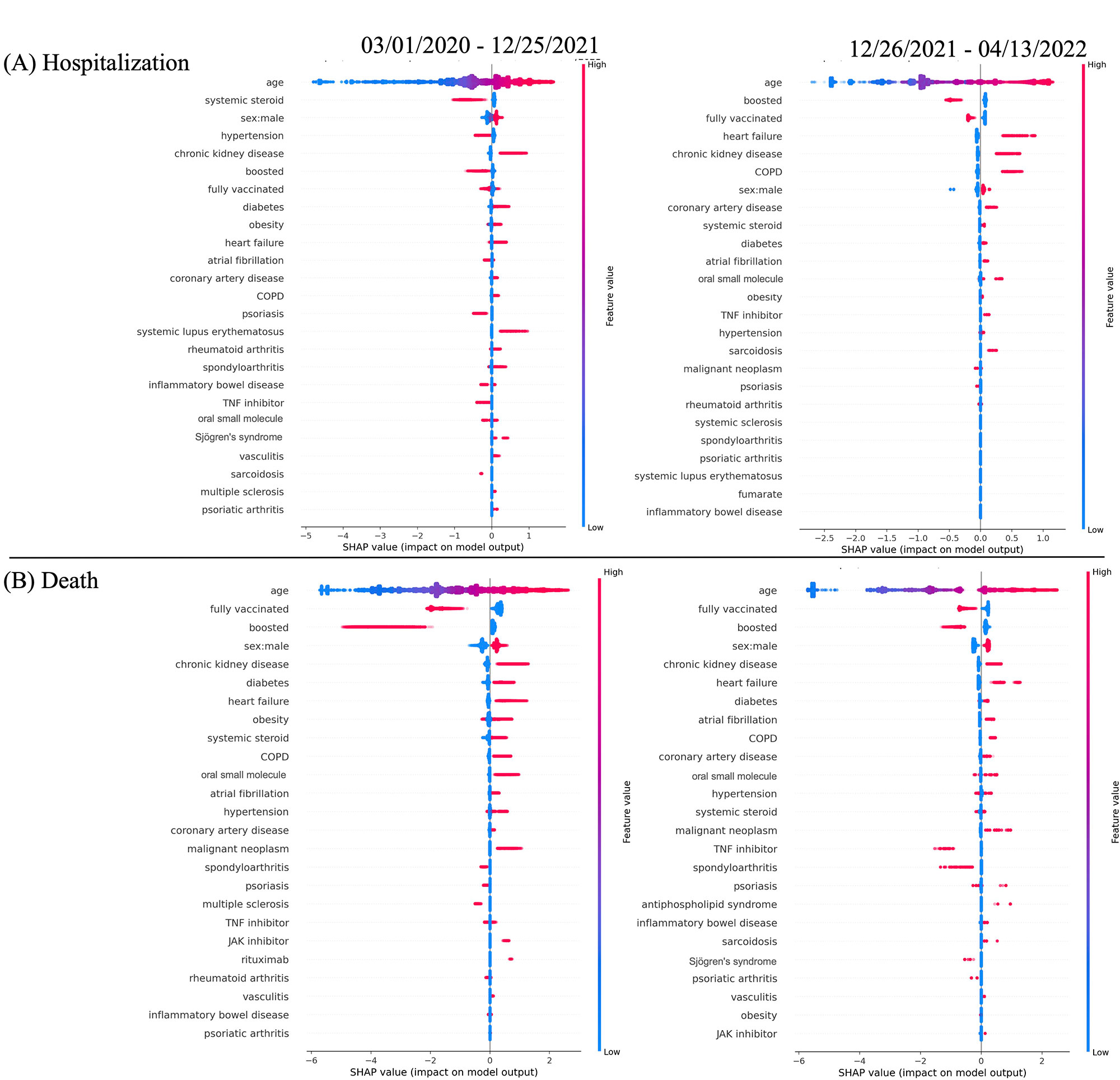
Results: In the pre-Omicron period, 1,476,322 people were tested with 11% positive. Of these, 2.5% were hospitalized and 3.2% died. 78,061 IMID pts were tested with 7.9% positive, and of these 3% were hospitalized and 4.5% died, higher rates than the overall population. The rheumatologic IMIDs had greater hospitalization and mortality rates compared to other IMIDs. In the Omicron period, the positive rate increased (21.9%) but the percentage hospitalized (0.8%) and dying (1.8%) decreased, partly due to increased vaccination status and possibly decreased viral virulence. In both time periods, pts with IMIDs had an increased rate of hospitalization and death compared to non-IMID pts (Tab 1). XGBoost models achieved AUROC 0.74 – 0.91 on the test set. Age and multiple comorbidities were strongly associated with an increased risk of hospitalization and death, whilst vaccination and booster status were strongly associated with a decreased risk of hospitalization and death. Pts with IMIDs overall had higher percentages of hospitalization and death than those without, likely associated with age and comorbidities. However, few IMIDs were associated with severe outcomes, and those had low feature importance (Figs 1, 2). Spondyloarthritis and Sjögren’s were less associated with death, as was the use of TNFi. The favorable or unfavorable association of specific IMIDs and treatments with outcomes varied by time period and analytic method (Figs 1, 2).
Conclusion: Pts with IMIDs, especially rheumatologic, experienced more severe outcomes than non-IMID pts. Most immunomodulatory medications were not associated with increased risk. Some IMIDs and treatments were associated with decreased risk of severe outcomes, such as spondyloarthritis and Sjögren’s, as well as the use of TNFi. Certain drug classes may be weakly associated with increased risk but due to the inconsistency of this signal with different analytic methods and time periods, these observations need further research.
To cite this abstract in AMA style:
Mease P, Wei Q, Chiorean M, Iles-Shih L, Matos W, Baumgartner A, Molani S, Hwang Y, Belhu B, Hadlock J. Risk Factors for Severe COVID-19 Outcomes: A Study of Immune-mediated Inflammatory Diseases, Immunomodulatory Medications, Vaccination Status, and Comorbidities in a Large US Healthcare System [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/risk-factors-for-severe-covid-19-outcomes-a-study-of-immune-mediated-inflammatory-diseases-immunomodulatory-medications-vaccination-status-and-comorbidities-in-a-large-us-healthcare-system/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-severe-covid-19-outcomes-a-study-of-immune-mediated-inflammatory-diseases-immunomodulatory-medications-vaccination-status-and-comorbidities-in-a-large-us-healthcare-system/