Session Information
Date: Tuesday, November 14, 2023
Title: (2039–2060) Pediatric Rheumatology – Clinical Poster III: Potpourri
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Among adults who develop SARS-CoV-2 infection, those with rheumatic diseases (RDs) have similar hospitalization rates compared to those without RDs. Similar comparisons are lacking in children, due to the overall rarity of hospitalization due to SARS-CoV-2 in this population. We aimed to examine hospitalization risk for SARS-CoV-2 in pediatric patients with rheumatic diseases and its associated risk factors.
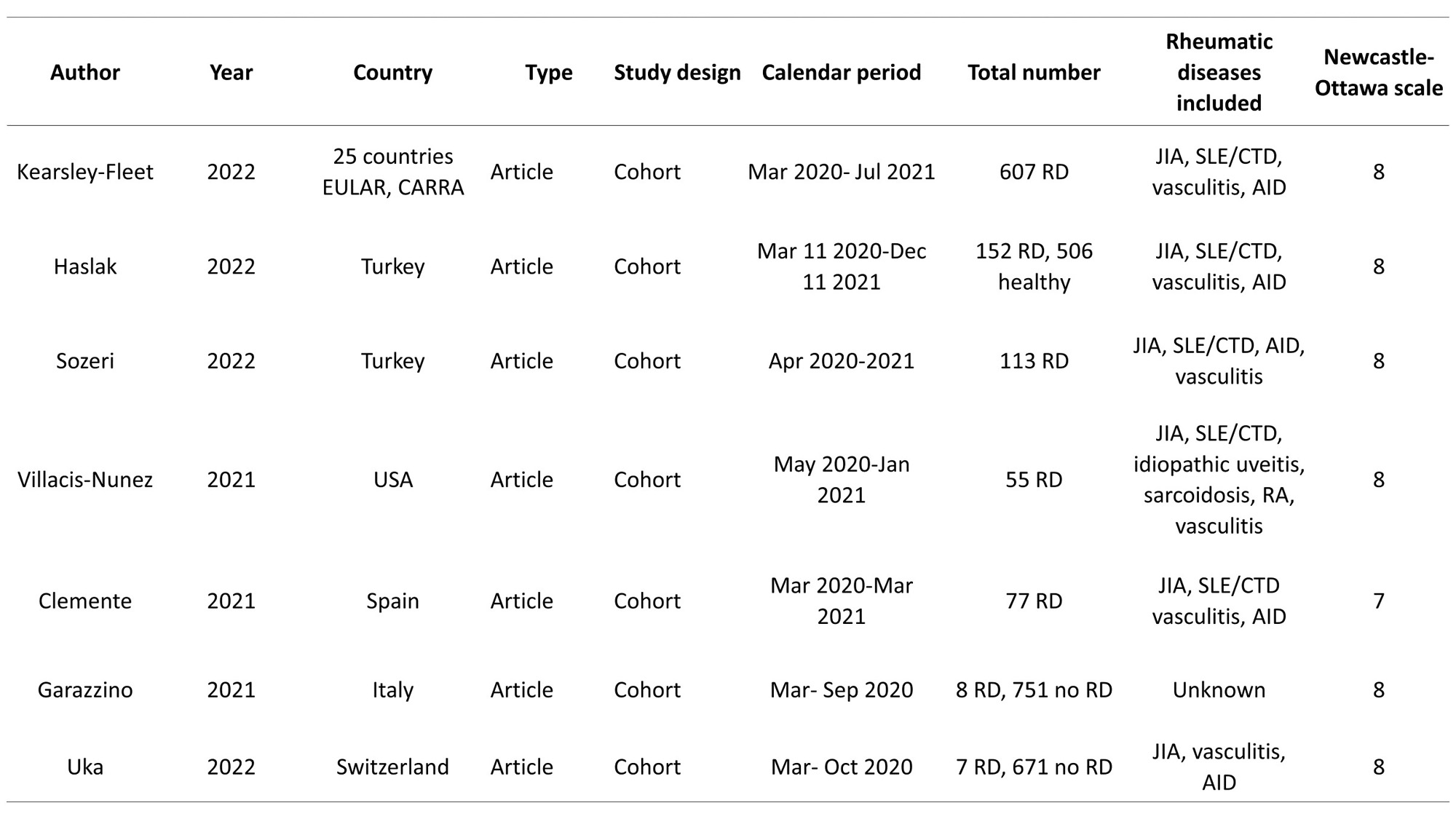
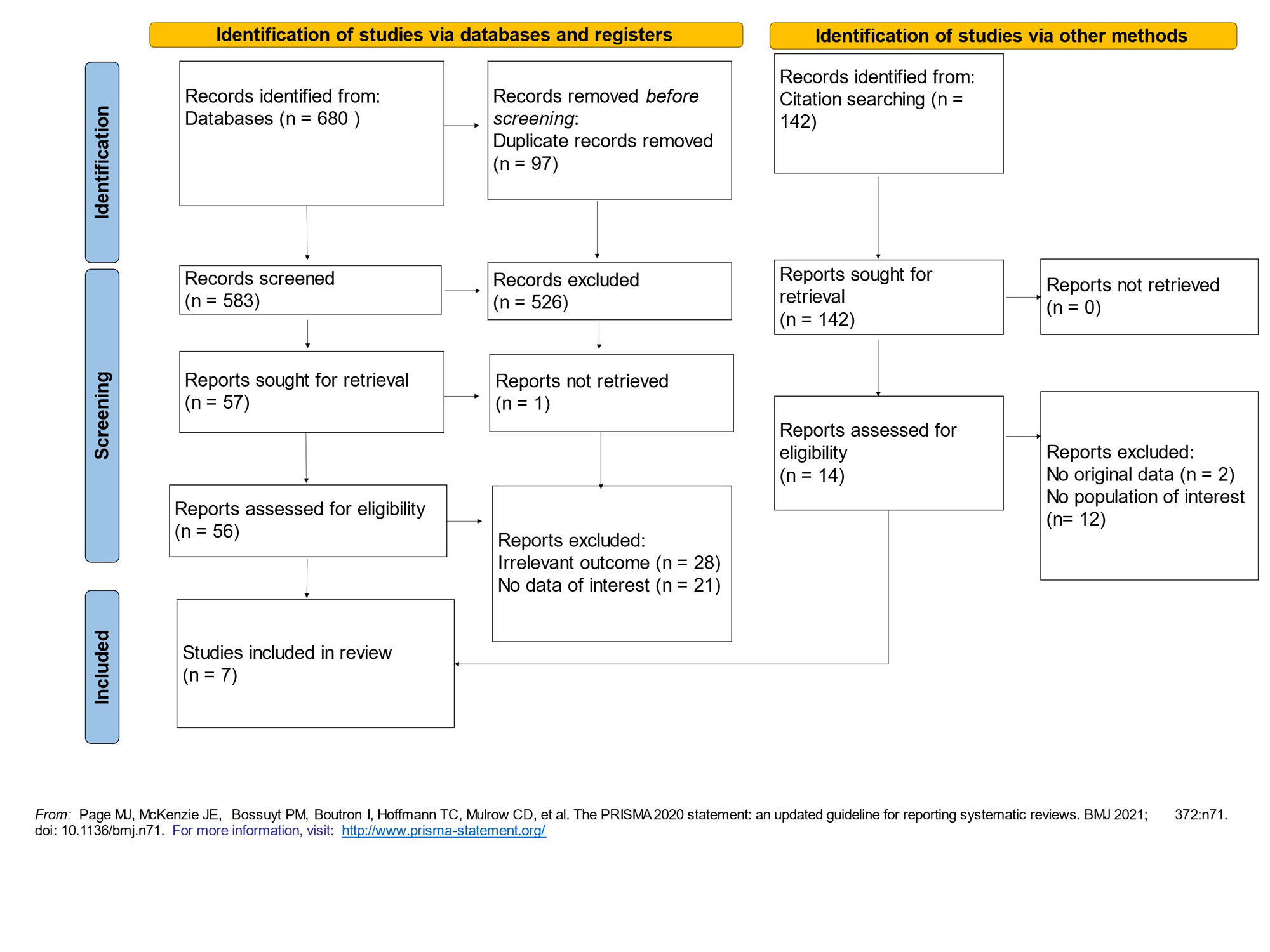
Methods: We conducted a systemic literature search in MEDLINE, EMBASE, Web of Science, and China National Knowledge Infrastructure from December 1, 2019 through April 20, 2023. We included observational studies of pediatric rheumatic disease populations with sufficient data to calculate at least one odds ratio (ORs) for the primary outcome of COVID-19-related hospitalization(Fig 1). We assessed risk of bias using the Newcastle-Ottawa Scale for cohort studies. Study heterogeneity was assessed by Q statistics and I2 statistic. ORs with 95% confidence intervals (95% CIs) were calculated using fixed-effect models based on the Mantel-Haenszel method if I2 < 50%.
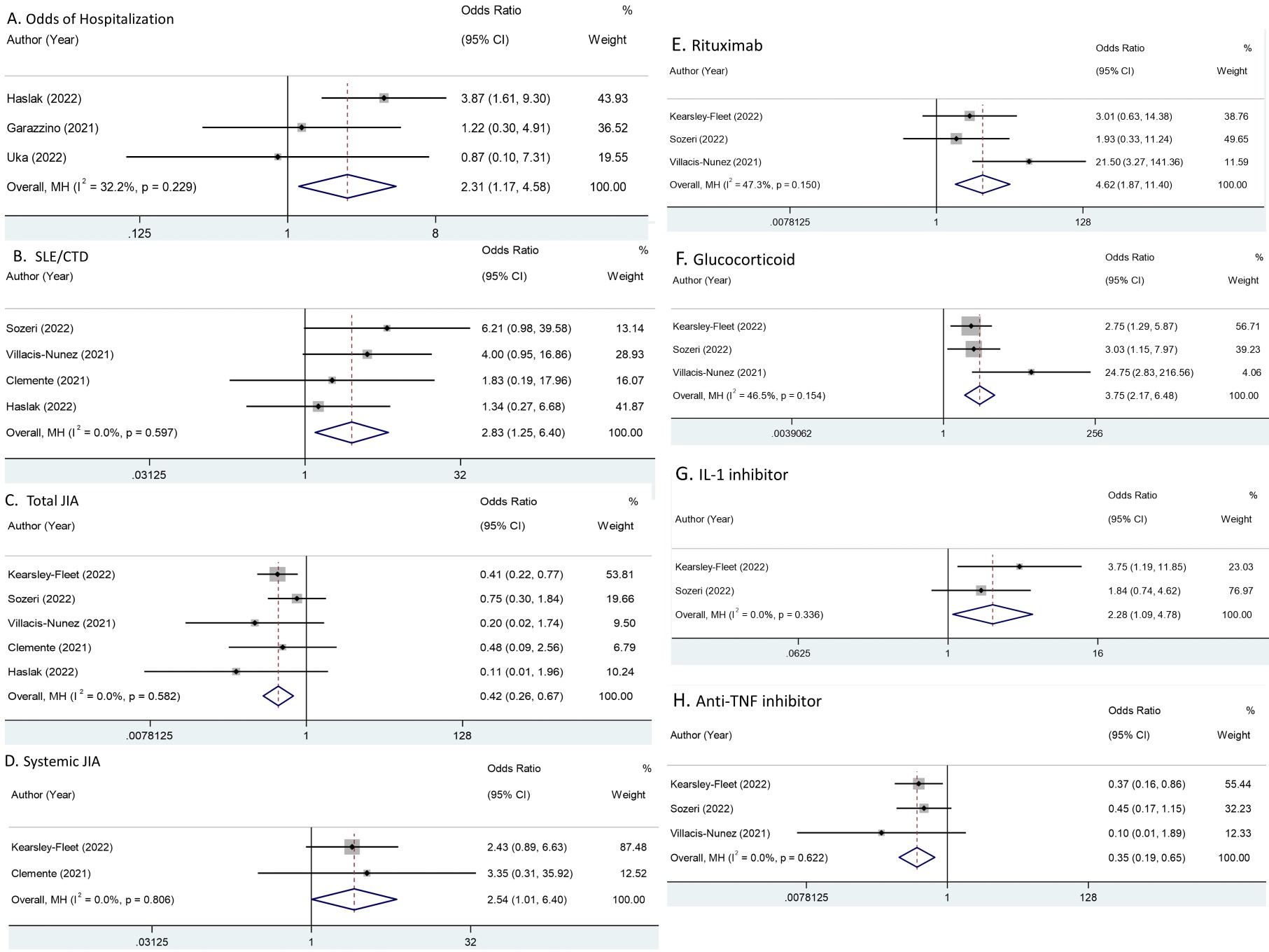
Results: Sevencohort studies capturing 1,019 pediatric RD patients with confirmed SARS-CoV-2 were included (Table 1, Fig 1). Odds of hospitalization was increased in children with RD compared to healthy children ((OR 2.31; [95% CI, 1.17-4.58]), Fig. 2A). The diagnoses of systemic lupus erythematosus/connective tissue disease (SLE/CTD) ((OR 2.83; [95% CI 1.25, 6.40), Fig. 2B) and systemic juvenile idiopathic arthritis (JIA) ((OR 2.54, [95% CI, 1.01-6.40]), Fig. 2D) were associated with increased odds of hospitalization, while total JIA was associated with reduced odds ((OR 0.42, [95% CI, 0.26-0.67]), Fig. 2C). Use of rituximab ((OR 4.62, [95% CI, 1.87-11.4], Fig. 2E)), glucocorticoids ((OR 3.75; 95% CI [2.17-6.48]), Fig. 2F) or IL-1 inhibitors ((OR 2.28, [95% CI, 1.09-4.78], Fig. 2G) was associated with increased odds of hospitalization; use of TNF inhibitors was associated with reduced odds ((OR 0.35, [95% CI, 0.19-0.65], Fig. 2H). Use of tocilizumab (OR 0.99, [95% CI, 0.34-2.87]), tofacitinib (OR 3.01, [95% CI, 0.69-13.12]) and traditional DMARDs (OR 0.71, [95% CI, 0.43-1.17] were not associated with a change in odds of hospitalization. A limitation of the study was the predominantly Caucasian population, with no data for patients from China, India, Korea or Japan.
Conclusion: Pediatric patients with RDs have higher oddsof SARS-CoV-2 related hospitalization than healthy children, especially those with SLE/CTD and those using Rituximab, glucocorticoids and IL-1 inhibitor.In contrast, JIA and anti-TNF inhibitor use was associated with a reduced odds of hospitalization.
To cite this abstract in AMA style:
Zhao Q, Wallace B, Jung L, Ronis T. Risk Factors for Hospitalization for SARS-CoV-2 in Pediatric Patients with Rheumatic Diseases: A Systematic Review and Meta-analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/risk-factors-for-hospitalization-for-sars-cov-2-in-pediatric-patients-with-rheumatic-diseases-a-systematic-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-hospitalization-for-sars-cov-2-in-pediatric-patients-with-rheumatic-diseases-a-systematic-review-and-meta-analysis/