Session Information
Date: Sunday, November 5, 2017
Title: Education Poster
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Subspecialty consults in a hospital setting often contribute to disjointed patient care and frustrated providers. Miloslavsky et al (1) previously demonstrated improvement in rheumatology fellows’ ability to teach in a consult setting in a standardized learner environment. We sought to perform a similar intervention in a pilot real-world setting at our two teaching hospitals. Our goals were to improve fellows’ ability to teach, create interest in the field, and facilitate more collaborative patient care.
Methods:
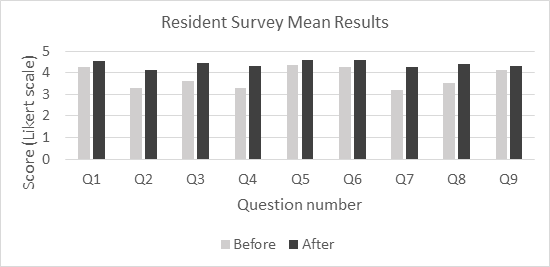
A 10-question pre-intervention survey was administered to residents on internal medicine teams at each of the 2 training hospitals. The survey utilized a 5-point Likert scale to address 7 aspects of rheumatology fellows’ ability to teach, overall effectiveness and approachability, as well as quantifying percentage of time recommendations were shared in person. Our intervention included: a workshop for fellows on adult learning theory and self-directed learning; provision of pocket card containing medicine team locations, contact numbers, and prompt questions; monthly email reminders of the project goals to attendings and fellows. Rheumatology attendings standardized consult rounds by visiting teams following patient evaluations to relay our recommendations; fellows were instructed to lead the discussion. We employed this strategy for four months, after which the same survey was administered to residents on medicine teams. There was no randomization or blinding due to the nature of the study.
Results:
There were 33 pre-intervention and 15 post-intervention completed surveys. Mean scores on each of the 10 questions improved from pre- to post-intervention. Overall teaching effectiveness improved from mean of 3.55 to 4.4 (on 5-point scale). Prior to the intervention, 9% of respondents reported receiving in-person recommendations at least 50% of the time compared to 60% of respondents after the intervention.
Conclusion:
The findings of our pilot project are similar to the “Rheumatology Fellows as Teachers” project by Miloslavsky et al (1). With a simple teaching intervention and standardization of the workflow, we improved perceived teaching skills in all areas measured. Our limitations included few survey respondents and inability to control for improvements in fellow teaching due to increased experience. Despite these limitations, our findings suggest that having a standardized process for consultation that fosters a positive teaching interaction and collaboration can have far reaching effects on resident fellow interactions as well as patient care. Future studies could include other consult services, and a paired pre- and post-intervention analysis.
1. Miloslavsky, E. M., et al (2016), Fellow As Teacher Curriculum: Improving Rheumatology Fellows’ Teaching Skills During Inpatient Consultation. Arthritis Care & Research, 68: 877–881.
To cite this abstract in AMA style:
Smith H, Kazzaz S, Mohan A, Barnes J. Rheumatology Fellows Teaching in a Consult Setting: Pilot Project at Two Training Hospitals [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/rheumatology-fellows-teaching-in-a-consult-setting-pilot-project-at-two-training-hospitals/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatology-fellows-teaching-in-a-consult-setting-pilot-project-at-two-training-hospitals/