Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: SLE is a leading cause of mortality in young adults, particularly in those identifying as Black or Hispanic or who are socioeconomically disadvantaged. These populations may also experience differential access to lupus care and care quality, which could contribute to existing outcome disparities. Thus, we sought to examine potential disparities in markers of lupus care access and quality in a uniformly insured, national cohort of young adults with lupus who are at particularly high risk for poor outcomes. The objective of this study was to compare visit-based retention in lupus care (marker of access) and receipt of serologic testing (marker of quality) by race and ethnicity, neighborhood socioeconomic disadvantage, and geography.
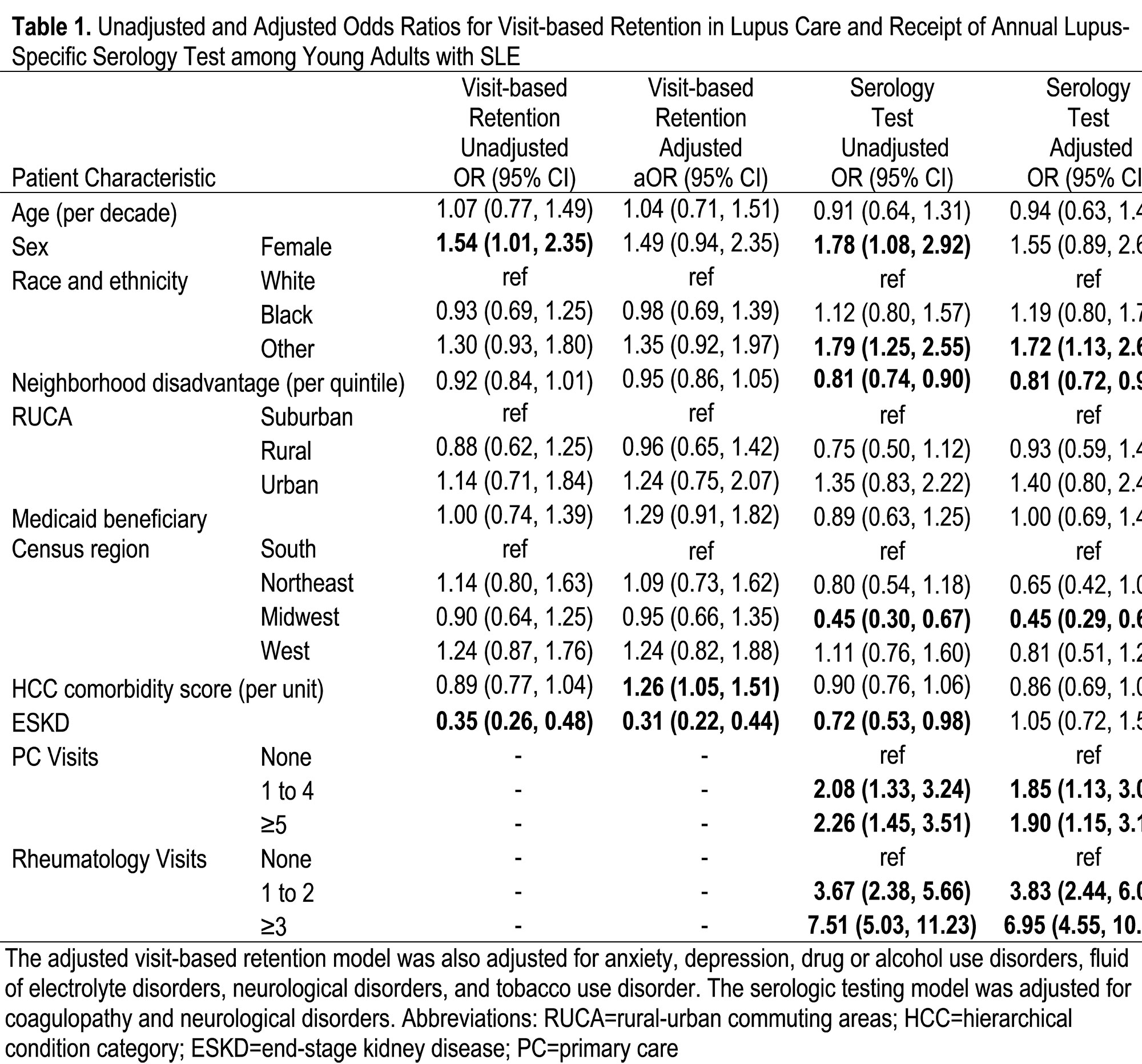
Methods: This cohort study analyzed a geo-linked 20% national sample of young adult (ages 18-35) Medicare beneficiaries. Inclusion required a hospitalization, rheumatology physician visit, or two other non-hospitalization encounters at least two months apart that were associated with a lupus diagnosis code between January 1, 2013 and June 30, 2014 (98% specificity, 85% sensitivity). Patients had to have 18 months of claims. The first six months were used to establish comorbid conditions. Rheumatology visits and serologic testing were evaluated in a subsequent 12-month assessment period. Visit-based retention in lupus care was defined as a rheumatology visit in both six-month periods of the assessment period. Serologic testing was defined as at least one complement or dsDNA test within the 12 months. Patients were categorized into US census region, quintile of neighborhood disadvantaged based on Area Deprivation Index, and rural, suburban, or urban area. Multivariable logistic regression models were fit for retention and serologic testing.
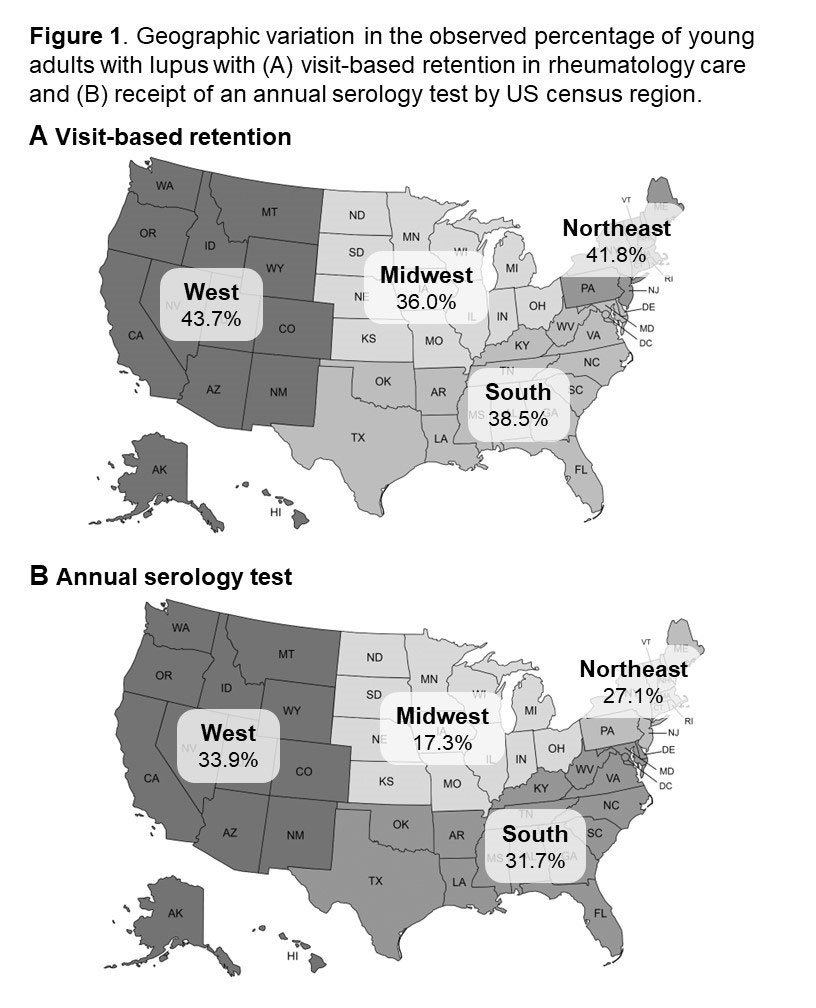
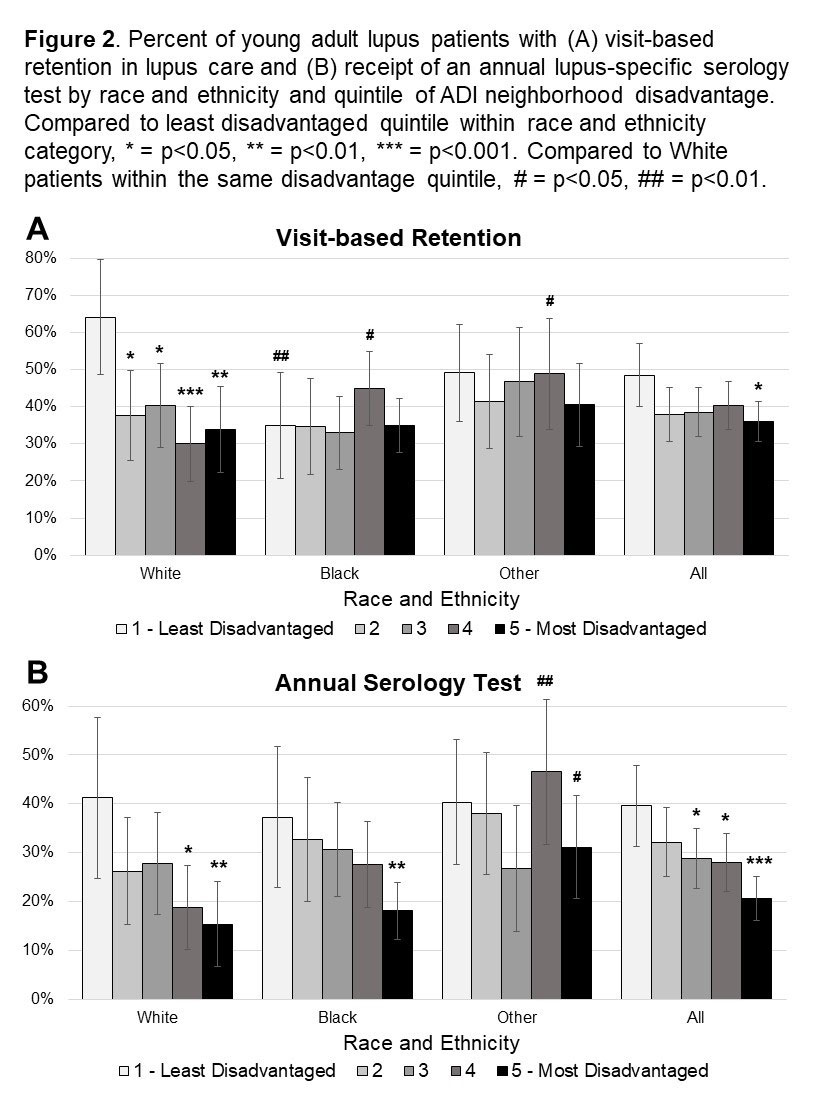
Results: Among 1,036 young adults with lupus (mean age 29), 39% (95% CI 36-42%) had visit-based retention in lupus care, and 28% (95% CI 26-31%) had serologic testing. Both visit-based retention and serologic testing was lowest in the Midwest and highest in the West (Figure 1). No differences were found by rural, suburban, or urban area. White beneficiaries from the least disadvantaged quintile of neighborhoods had ≥15% higher visit-based retention than other beneficiaries (64 vs 30-49%; Figure 2). Serologic testing was lower with higher neighborhood disadvantage (Figure 2), decreasing 19% for each quintile increase in neighborhood disadvantage (aOR 0.81; 95% CI 0.72, 0.91; Table 1). Visit-based retention but not serologic testing, increased with higher comorbidity burden. Presence of primary care visits increased odds of serologic testing two-fold, while rheumatology visits were the strongest predictor (aOR 3.83; 2.44, 6.01).
Conclusion: In this cohort of young adults with lupus, only 39% saw a rheumatologist at least once each six months and fewer than one in three had an annual serologic test. Despite uniform Medicare coverage, disparities in markers of lupus care access and quality were identified by neighborhood disadvantage, race and ethnicity, and region. These findings suggest further research is needed to evaluate additional lupus care quality indicators and how such care differences may impact lupus outcome disparities in the US.
To cite this abstract in AMA style:
Schletzbaum M, Powell W, Garg S, Kramer J, Astor B, Gilmore-Bykovskyi A, Kind A, Bartels C. Retention in Rheumatology Care and Receipt of Lupus-Specific Serologic Testing Among Young Adults with Systemic Lupus Erythematosus: A Medicare Cohort Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/retention-in-rheumatology-care-and-receipt-of-lupus-specific-serologic-testing-among-young-adults-with-systemic-lupus-erythematosus-a-medicare-cohort-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/retention-in-rheumatology-care-and-receipt-of-lupus-specific-serologic-testing-among-young-adults-with-systemic-lupus-erythematosus-a-medicare-cohort-study/