Session Information
Date: Saturday, November 6, 2021
Title: Sjögren's Syndrome – Basic & Clinical Science Poster (0296–0322)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Renal disease in primary Sjogren’s syndrome (pSS) can occur in form of tubulointerstitial nephritis (TIN) or glomerulonephritis (GN). Data from India on pSS is sparse and that on nephritis is even less. Thus, we studied the prevalence and impact of renal disease on patient outcomes.
Methods: Retrospective review of 179 (F:M 12.7:1, age 41.7±12.9 years) patients of pSS (ACR 2016 criteria) was carried out from electronic health records at a single centre from 2000 to 2020. Data on nephritis and other clinical and laboratory variables was collected from baseline visit. Outcomes studied were chronic kidney disease (CKD) and death. Multivariate logistic regression was used to identify predictors. Linear mixed effects models were used to predict rise in creatinine on follow up. Kapan Meier survival analysis was undertaken for a composite outcome of death or CKD.
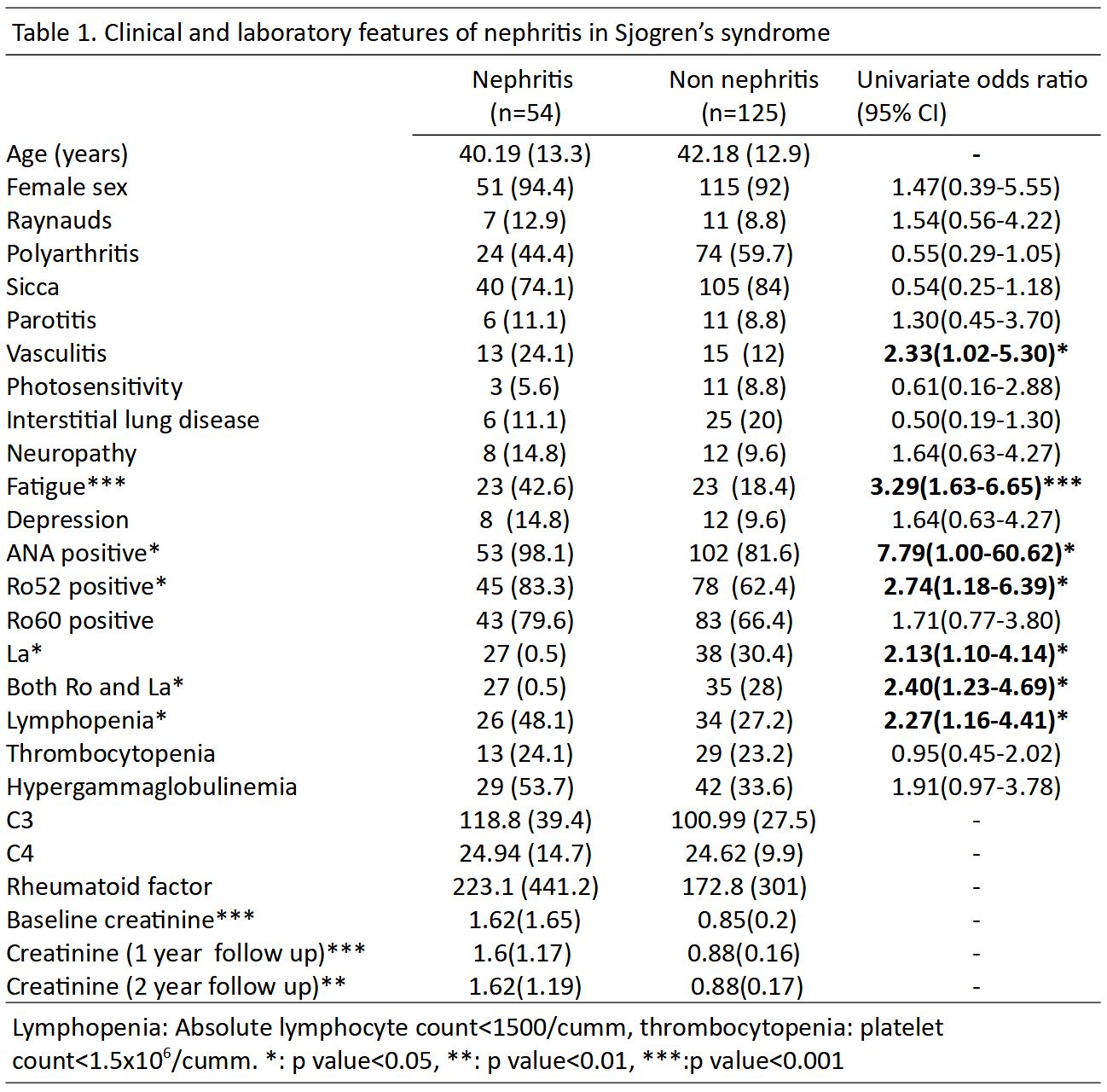
Results: Among 179 patients with pSS 54 (30.17%) patients had nephritis. Their mean age was 40.19 (13.28) years and they had 157.3 person years follow up. 26 of these 54 patients presented with hypokalemic paralysis (Table 1). Of the 10 renal biopsies, TIN was present in 8 and mesangioproliferative GN in 2.
Vasculitis (OR 2.33), fatigue (OR 3.29), ANA positivity (OR 7.79), anti-Ro52 (OR 2.74), anti-La (OR 2.13), both Ro and La (OR 2.4) and lymphopenia (OR 2.27) were associated with nephritis on univariate analysis. On multivariate analysis, only fatigue (OR 2.83) and an interaction between polyarthritis and vasculitis (OR 9.17) was associated with nephritis.
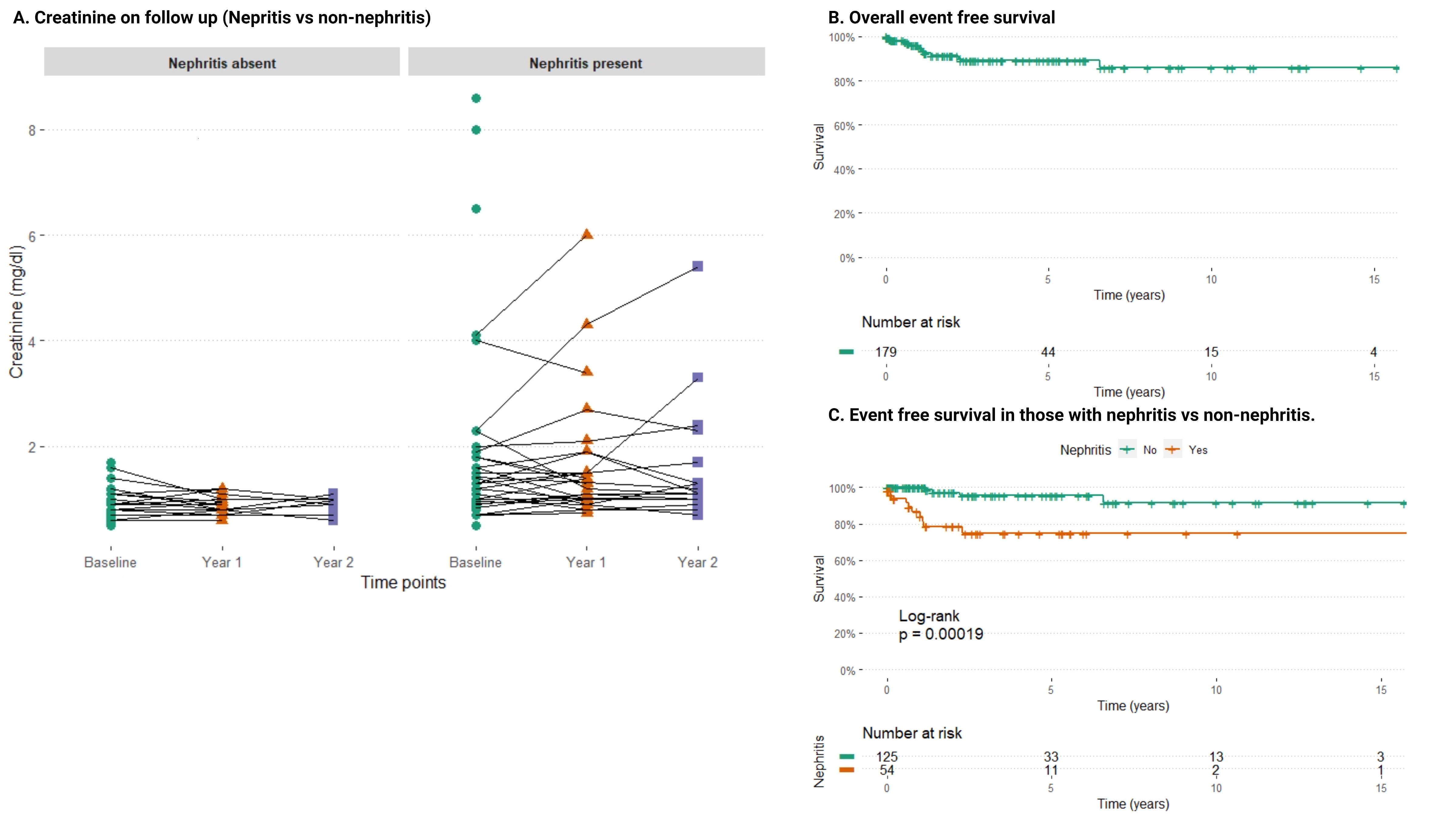
Creatinine at 1 year (1.6±1.17 vs 0.8±0.2) and 2 years (1.62±1.19 vs 0.8±0.2) follow-up was higher in the nephritis group than those without nephritis (Figure 1a). Adjusted for immunosuppression used, baseline hematuria, leucocyturia, 24 hour urinary protein and thrombocytopenia were independent predictors of rise in creatinine on follow up. Six patients died and 10 patients developed CKD. Event (death or CKD) free survival was 89.1% at 5 years (Figure 1b). Patients with nephritis had worse event free survival as compared to those without nephritis (Figure 1c).
Conclusion: In our cohort almost 1/3rd had nephritis and its presence lead to higher probability of death or CKD.
To cite this abstract in AMA style:
Chatterjee R, Balakrishnan A, Kharbanda R, Rathore U, Gupta L, Misra D, Agarwal V, Aggarwal A, Lawrence A. Renal Involvement in Sjőgren’s Syndrome: Predictors and Impact on Patient Outcome [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/renal-involvement-in-sjogrens-syndrome-predictors-and-impact-on-patient-outcome/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-involvement-in-sjogrens-syndrome-predictors-and-impact-on-patient-outcome/