Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with lupus nephritis (LN) have a 9-fold higher risk of cardiovascular disease (CVD), highlighting the urgent need to target CVD prevention. Studies in IgA nephropathy and transplant report that severe renal arteriosclerosis (ASCL) on biopsies is an early predictor of CVD. We previously reported a high burden of renal ASCL, accelerated by two decades in LN patients compared to healthy peers. We saw 80% positive predictive value of reported ASCL, but 50% of pathology reports overlooked renal ASCL in LN biopsies due to lack of standard systematic reporting of vascular lesions. Therefore, we aimed to examine whether overlooked renal ASCL was partially responsible for the prior negative studies on renal ASCL and CVD in LN. We hypothesized that renal ASCL would be an early predictor of CVD in LN when over-read pathology and reports were incorporated.
Methods: We identified all LN patients who underwent a kidney biopsy 1994-2017 at an academic center using a comprehensive native renal biopsy database. Data included socio-demographics and pathology reports from the first renal biopsy. SLE diagnosis was validated using ACR and SLICC 2012 criteria. CVD events were validated using American Heart Association guidelines. At the time of kidney biopsy, chronic kidney disease (CKD) stage and atherosclerotic cardiovascular disease (ASCVD) risk factors were recorded. Pathology reports were reviewed for reported renal ASCL, classified using Banff donor kidney biopsy ASCL grading: none, mild, moderate or severe. A blinded pathologist over-read 25% of biopsies using Banff ASCL grading. When pathology reports lacked any comment on the presence or absence of renal ASCL, we supplemented the over-read renal ASCL grade. Multivariable logistic regression examined relationships with CVD events.
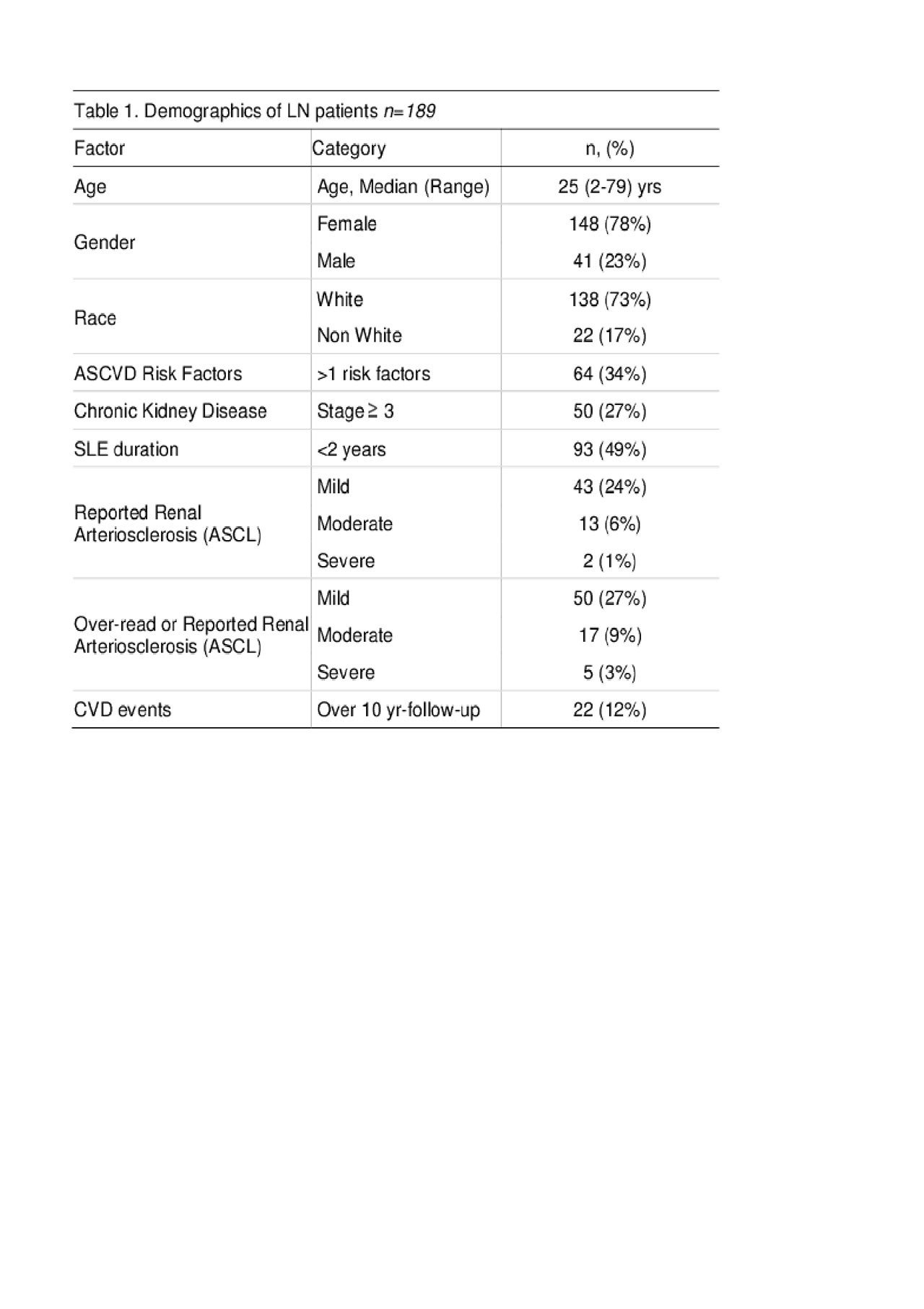
Results: Among 189 incident LN patients with kidney biopsies, 78% were female, 78% white and the median age was 25 (2-79), 27% had ≥ 3 CKD stage and 34% had >1 ASCVD risk factors. Overall, 32% had any and 7% had moderate-severe reported renal ASCL. The prevalence of any and moderate-severe by reported or over-read renal ASCL was 38% and 12% (Table 1). We found 22 CVD events from 1 year before LN through 10 years of follow-up, comparable to published rates in LN (12% vs 11%, p 0.9).
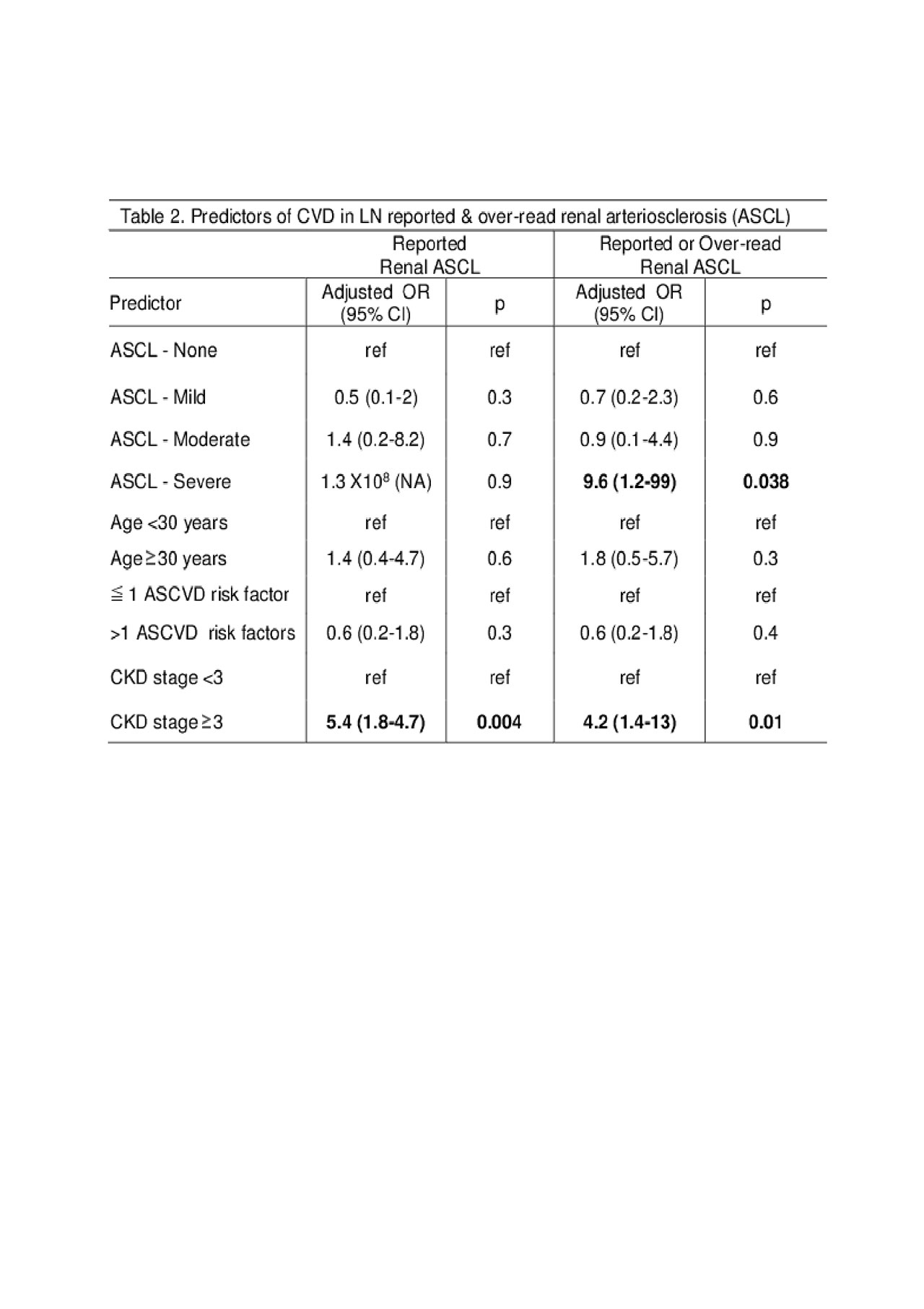
In the group with reported renal ASCL, multivariable analyses showed that ≥ 3 CKD stage increased risk of CVD by 5-fold (Adjusted OR 5.4, CI 1.8-18, p 0.004; Table 2) but reported renal ASCL was not a predictor of CVD. However, examining reported or over-read renal ASCL, multivariable analysis showed that severe renal ASCL at LN diagnosis increased risk of CVD by 10-fold compared to those without ASCL (OR 9.6,CI 1.2-99, p 0.038). CKD stage ≥ 3 remained a predictor; >1 ASCVD risk factors and age were not predictors.
Conclusion: Systematic grading and reporting of renal ASCL in at first LN biopsy is critical, because severe renal ASCL can predict CVD in LN patients. In future studies, we recommend over-reading all biopsies to grade renal ASCL and examining CVD associations in diverse LN cohorts.
To cite this abstract in AMA style:
Garg S, Panzer S, Hansen K, Plafkin C, Smith M, Bartels C. Renal Arteriosclerosis Predicts Cardiovascular Disease in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/renal-arteriosclerosis-predicts-cardiovascular-disease-in-lupus-nephritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/renal-arteriosclerosis-predicts-cardiovascular-disease-in-lupus-nephritis/