Session Information
Session Type: Poster Session A
Session Time: 6:00PM-7:00PM
Background/Purpose: Uncontrolled uveitis can lead to visual complications in 50% of children with JIA associated uveitis (JIA-U). While arthritis and uveitis are not considered to run parallel courses, recent studies report that children with active arthritis may have concurrent uveitis1. Further, as subclinical synovitis can be detected by musculoskeletal US (MSUS), findings of active arthritis by MSUS may better reflect disease activity and have implications for uveitis activity2. This retrospective study aims to evaluate the temporal association between arthritis and uveitis in patients with JIA-U, and whether this association varies when arthritis is detected by MSUS versus clinical examination.
Methods: Medical charts of children with JIA-U who had an ophthalmology examination within 6 weeks, either 3 weeks before or after a rheumatology examination (clinical and/or MSUS) were reviewed. Participants were able to contribute more than one visit. Active uveitis was defined as anterior chamber (AC) inflammation grade of ≥0.5+ cells as per the Standardization of Uveitis Nomenclature Working Group criteria. Active arthritis was defined by 1) joint swelling, or in the absence of joint swelling, limited range of motion in a joint with tenderness; or 2) abnormal MSUS as per OMERACT. Primary outcome was presence of active uveitis within 6 weeks of arthritis examinations.
Results: Eighteen patients contributed 49 total visits (Table 1). Active arthritis by either MSUS or clinical examination was documented in 32 visits and 10 (31%) of these visits also had evidence of active uveitis. Of the 17 visits with inactive arthritis, only 1 (6%) had active uveitis (Fig. 1).
When focusing on visits that had only a clinical examination (n=33) we found that 23 (70%) had active arthritis and that 7 of these 23 visits (30%) also had active uveitis. Of the 10 visits with inactive arthritis on clinical examination, none had active uveitis.
Of 16 visits with only an MSUS examination, 9 (56%) had active arthritis and 3 of these 9 also had uveitis (33%). Of the 7 visits with inactive arthritis by MSUS, only 1 (14%) had active uveitis.
Fifteen visits had both an MSUS and clinical examination documented (Fig. 2). Six of these visits (40%) showed arthritis on both examinations with 3 visits (50%) having uveitis also.
Conclusion: Our findings suggest that in children with JIA-U, an arthritis flare may be associated with a concurrent uveitis flare. Therefore, children with JIA-U who present with active arthritis may need an expedited ophthalmology examination. We found no significant difference between arthritis detection by clinical examination vs. MSUS in terms of uveitis activity. Future prospective studies with a larger population are required.
References 1. Liebling, E., et al. Temporal Relationship Between Juvenile Idiopathic Arthritis Disease Activity and Uveitis Disease Activity. Arthritis Care Res 2022;74:349–54.
2. Vega-Fernandez, P., et al. Ultrasonography in Pediatric Rheumatology. Rheum Dis Clin North Am 2022;48:217-31.
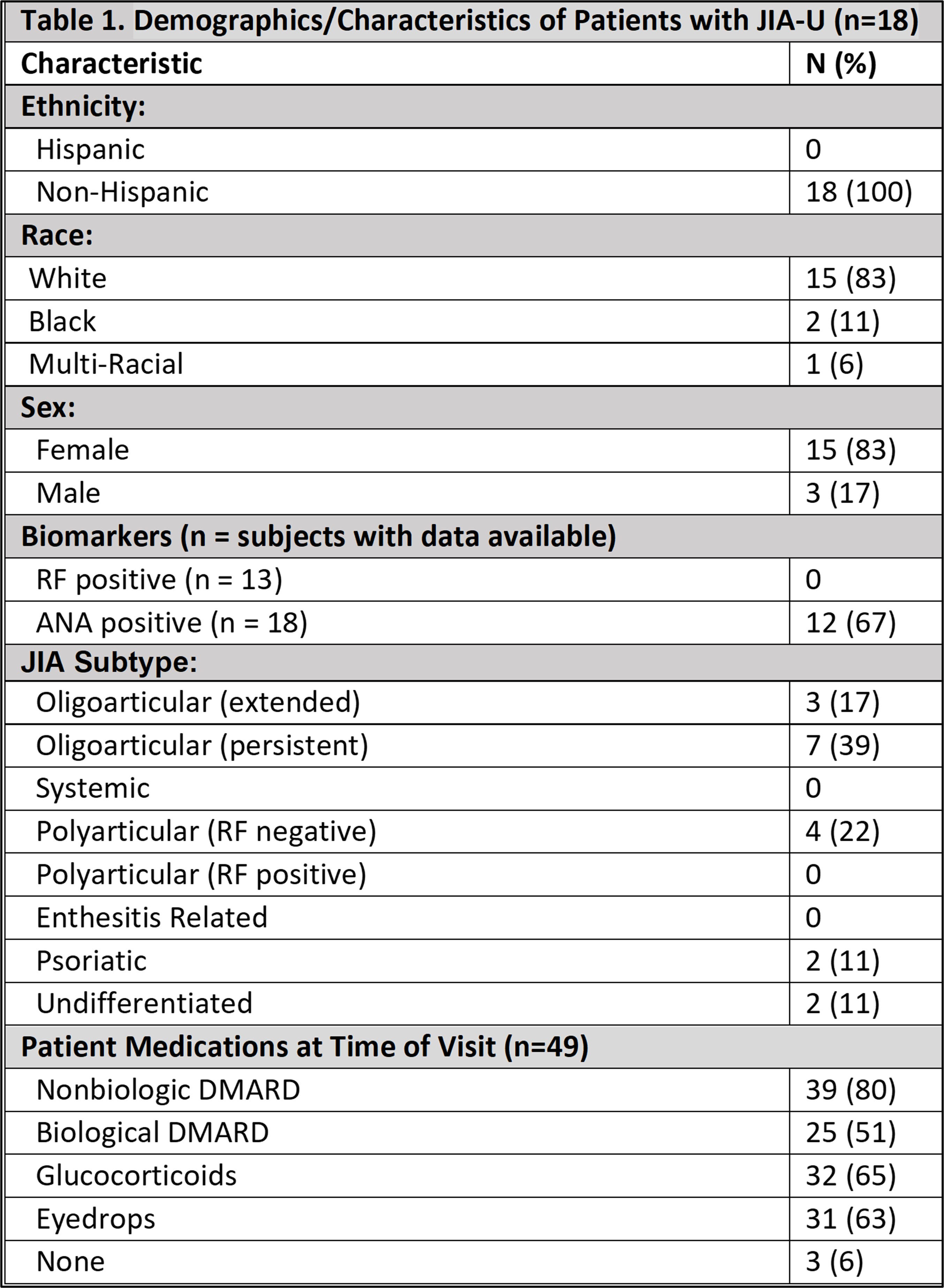 Table 1: Demographics/Characteristics of Patients with JIA-U
Table 1: Demographics/Characteristics of Patients with JIA-U
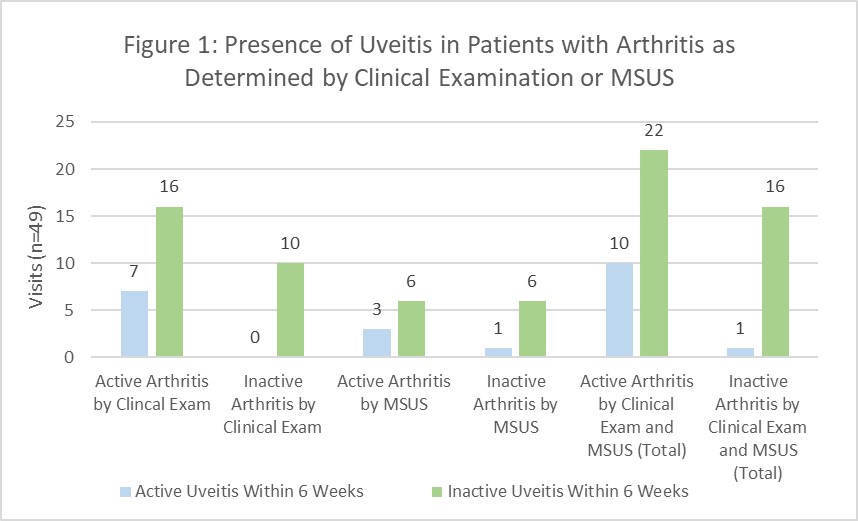 Figure 1: Presence of Uveitis in Patients with Arthritis as Determined by Clinical Examination or MSUS
Figure 1: Presence of Uveitis in Patients with Arthritis as Determined by Clinical Examination or MSUS
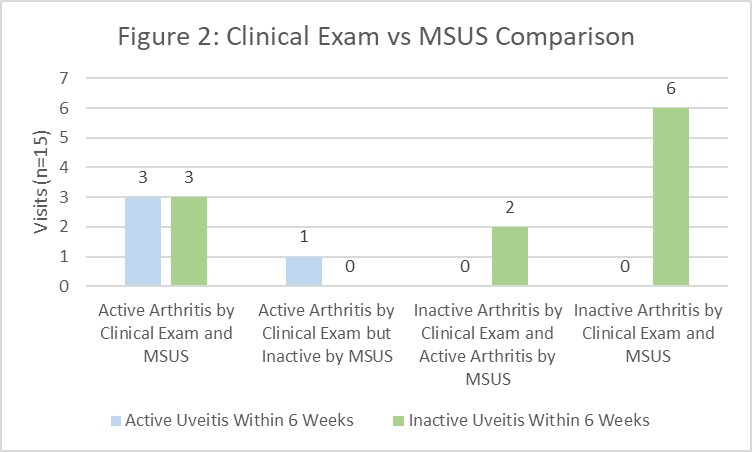 Figure 2: Clinical Exam vs. MSUS Comparison
Figure 2: Clinical Exam vs. MSUS Comparison
To cite this abstract in AMA style:
Karumuri M, Quinlan-Waters M, Duell A, Rogers K, Angeles-Han S, Vega-Fernandez P. Relationship Between Arthritis and Uveitis Disease Activity in Children with JIA [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/relationship-between-arthritis-and-uveitis-disease-activity-in-children-with-jia/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-between-arthritis-and-uveitis-disease-activity-in-children-with-jia/
