Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: SLE patients often experience relapse in the course of treatment, in spite of the progress of therapeutic strategy in SLE. The purpose of this study is to elucidate clinical features, outcome, and risk factors of relapse in patients with SLE who were newly diagnosed and treated at our hospital in recent 10 years.
Methods: This study is a retrospective cohort study. Newly diagnosed SLE patients who were treated in the department of Rheumatology, Fukushima Medical University hospital between 2011 and 2022 were collected. Patients who experienced relapse during observation period were regarded as Relapse-group (relapse was defined as BILAG grade B flare or more), and its clinical features including age, sex, disease duration, SLE symptoms, laboratory data and treatment such as the use of hydroxychloroquine (HCQ) and immunosuppressants (ISs), were compared with non-relapse SLE group. Cumulative relapse free survival in certain clinical items were also compared between the 2 groups using Kaplan-Meier curves.
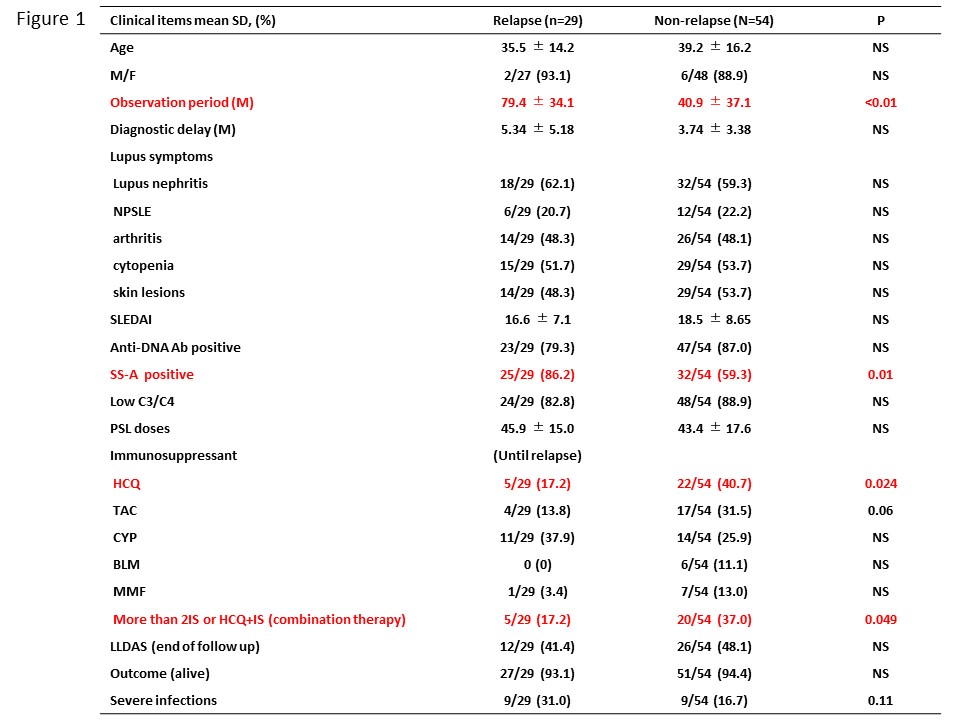
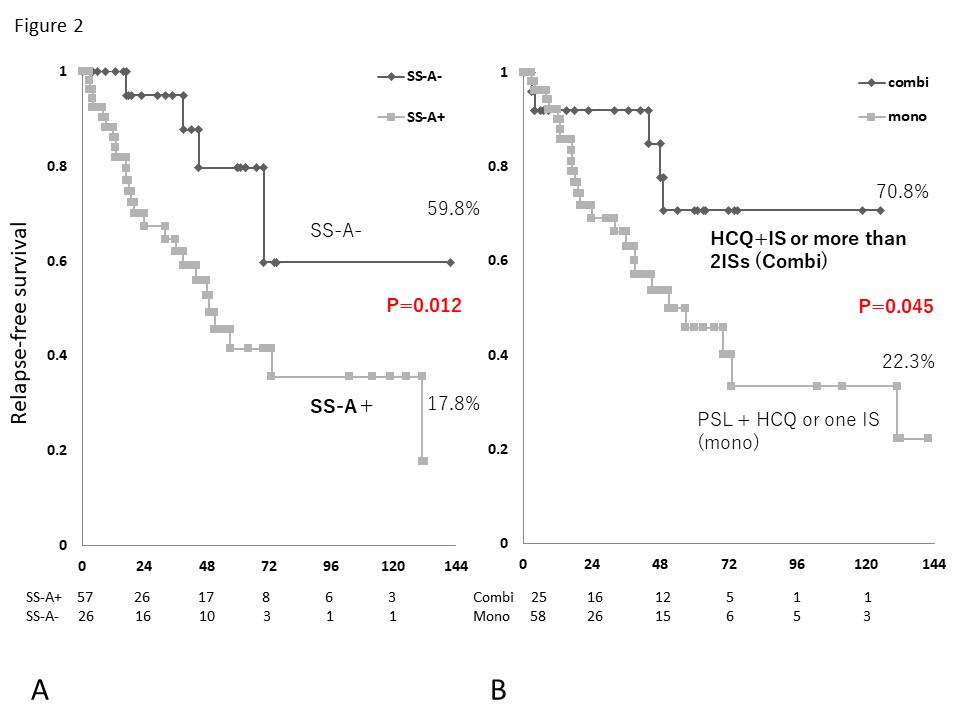
Results: Among 382 SLE patients who received treatment in our department from 2011 to 2022, 83 newly diagnosed SLE patients were included. The mean age was 37.9 years old, and 75 patients were female (90.4%). The mean SLEDAI scores were 17.8. In 83 patients, 29 patients experienced relapse during the study period. The comparison of clinical characteristics between Relapse group (29 patients) and Non-relapse group (54 patients) were shown in Figure 1. General characteristics were similar between the 2 groups including age, sex, SLE symptoms and serology tests except for observation period (p< 0.01) and anti-SS-A antibody positive (P=0.01). In therapy, significantly increased frequency of HCQ intake and combination immunosuppressive therapy (steroids and HCQ plus IS, or more than 2 ISs) were observed (P=0.024 and 0.049, respectively) in non-relapse group. Kaplan-Meier analysis showed significantly higher cumulative relapse-free survival in anti-SS-A negative group and combination immunosuppressive therapy group (P=0.012 and 0.045, respectively) (Figure 2).
Conclusion: Anti-SS-A positive, no HCQ use may be associated with SLE relapse in newly diagnosed SLE patients. Combination immunosuppressive therapy using steroids and HCQ plus IS, or more than 2 ISs may suppress new relapse of SLE in daily clinical practice.
To cite this abstract in AMA style:
Sato S, Yoshida S, Sumichika Y, Saito K, Matsumoto H, Temmoku J, Fujita Y, Matsuoka N, Asano T, MIGITA K. Relapse in Japanese Patients with Newly Diagnosed SLE and Its Clinical Characteristics in Daily Clinical Practice: A Single Center Experience in Recent 10 Years [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/relapse-in-japanese-patients-with-newly-diagnosed-sle-and-its-clinical-characteristics-in-daily-clinical-practice-a-single-center-experience-in-recent-10-years/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relapse-in-japanese-patients-with-newly-diagnosed-sle-and-its-clinical-characteristics-in-daily-clinical-practice-a-single-center-experience-in-recent-10-years/