Session Information
Date: Monday, November 13, 2023
Title: (1082–1099) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patient no-shows and late cancellations, defined as less than 24 hours from the visit, reduce operational efficiency, revenue generation, and lead to negative clinical outcomes. There has been an increasing trend in no-show and late cancellation rates at the University of Cincinnati Hoxworth rheumatology clinic. For fiscal year 2021, monthly rates ranged from 6.2-32.7%. Since each unused slot is not reimbursable, this has resulted in a negative financial impact. When extrapolated to all of Internal Medicine, this has led to a $2 million revenue loss. Previously, reminders for visits involved automated calls and mailing letters. Using Vizient clinical database to identify performance gaps, our smart aim was to integrate phone call reminders to decrease median benchmark for no-shows and late cancellation rates from 18.47% to 14.6% from October 31, 2022 to February 1, 2023.
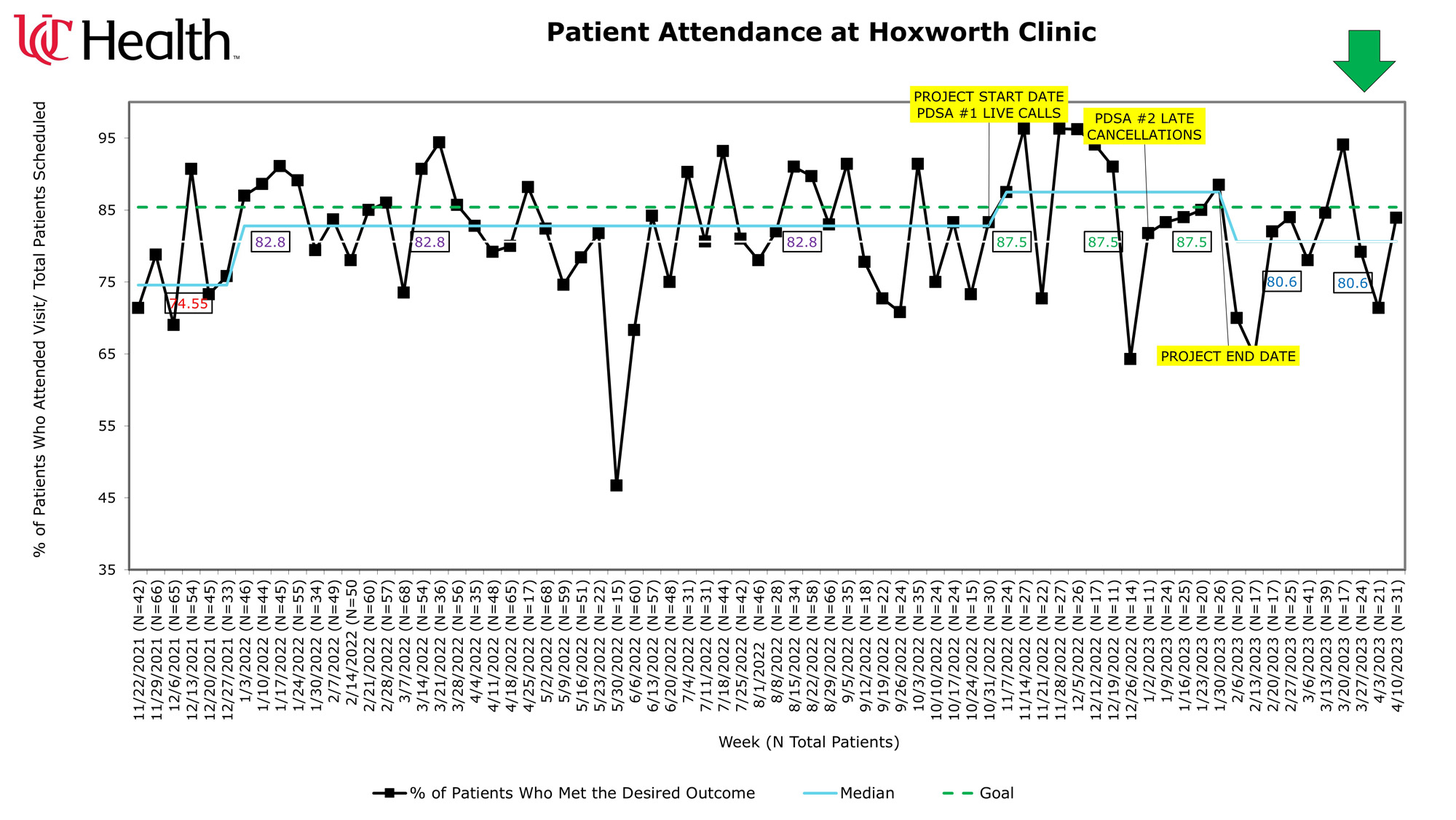
Methods: The 1st Plan-Do-Study-Act (PDSA) involved identifying the optimal lead time to call and was from October 31, 2022 to December 31, 2022. The 2nd aimed to refine phone call and messaging scripts and was from January 1 to February 1, 2023. Patients were called from 1 to 6 days prior to the visit. Alternate numbers or patient portals were used if they could not be reached. Conversations and barriers were documented in the medical record. To assess for common and special cause variations, baseline rates were plotted on a run chart starting from November 22, 2021 to April 14, 2023 (Figure 1).
Results: Monthly attendance ranged from 64.3-96.3% from October 31, 2022 to February 1, 2023 (N=11-30 patients per visit). The lowest rates were during Thanksgiving at 72.7% (N=22) and Christmas at 64.3% (N=14). Data for Thanksgiving and Christmas for 2021 were similarly low with median attendance of 74.55% (N=33-66). When excluding these holidays, the median rate was above the set benchmark of 85%. We concluded that low rates during holidays are special cause variations and can show positive shift if project is of a longer duration. After the project ended on February 1, 2023, rates dropped again below the benchmark to median of 80.6%. During PDSA #1 the optimal time to call was 5 to 6 days prior allowing for identification of barriers, some of which included transportation or work obligations. If barriers could not be resolved, patients on wait lists filled the open slots. During PDSA #2, late cancellations became increasingly higher than no-shows since they were unaware of the policy. There was a positive trend in attendance once scripts were refined to explicitly inform all patients of the policy. Also, phone calls were more effective than mailed letters or patient portal messaging due to the lead time and ability to identify barriers.
Conclusion: Monthly attendance ranged from 64.3-96.3% from October 31, 2022 to February 1, 2023. When excluding no-shows and late cancellations during Thanksgiving and Christmas, the median attendance rate was above the set benchmark of 85%. Low rates during holidays are special cause variations and can show positive shift if the next phase of the project is longer. The optimal time to call is 5 to 6 days prior and are opportunities to identify barriers and to fill open slots. There was a positive trend once scripts included explanation of the policy.
To cite this abstract in AMA style:
Jackson N, James M, Nguyen K, Vashisht P, Ware A. Reducing No-shows and Late Cancellations at an Academic Medical Center Subspecialty Clinic [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/reducing-no-shows-and-late-cancellations-at-an-academic-medical-center-subspecialty-clinic/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reducing-no-shows-and-late-cancellations-at-an-academic-medical-center-subspecialty-clinic/