Session Information
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: There are currently no clinical practice guidelines for monitoring RA-associated interstitial lung disease (RA-ILD). Pulmonary function tests (PFTs) and chest computed tomography (CT) imaging are among the most common tests utilized for RA-ILD surveillance, but the frequency of these tests in real-world settings is unclear. We examined real-world disease monitoring patterns in RA-ILD within the Veterans Affairs (VA) Health Care System, the largest integrated health care system in the U.S., from 1999-2021.
Methods: We performed a cohort study within national VA data warehouses, identifying individuals with RA-ILD (prevalent and incident) using validated algorithms that required multiple RA and ILD diagnostic codes (PPV >70%). The index date was the date patients fulfilled RA-ILD algorithm, and patients were followed for up to 7-years post-index date (reflecting the median survival in RA-ILD), censoring for death. Over the entire follow-up period and by sequential one-year intervals following the index date, we assessed completion of PFTs, chest CT imaging (any type), and outpatient visit frequency to rheumatology and pulmonology. PFTs, chest CTs, and outpatient visits (rheumatology and pulmonology) were obtained from VA administrative data and linked Centers for Medicare Services data. Vital status was determined from VA death records. Descriptive statistics were used to summarize RA-ILD monitoring patterns.
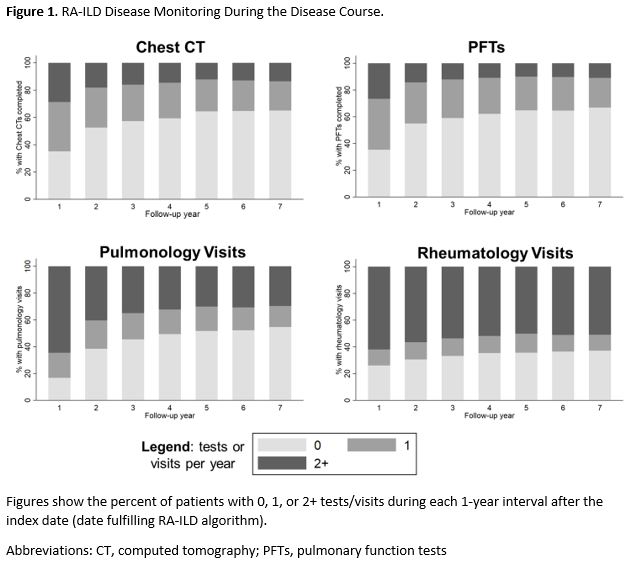
Results: We identified n=6,232 patients with RA-ILD (92.6% male, mean age 69.1 years). During follow-up, RA-ILD patients underwent monitoring with PFTs every 1.4 years (median [IQR] 0.5 [0.2, 1.0] tests/year) and chest CT imaging every 1.1 years (median 0.7 [0.3, 1.2] tests/year). PFT and CT monitoring frequency steadily decreased over the duration of disease, with PFTs or chest CTs being obtained in fewer than 50% of RA-ILD patients each year after the first year of follow-up (Figure 1). Among RA-ILD patients who did undergo PFTs or chest CTs during each 1-year interval, the majority had a single PFT or chest CT test during that year. Rheumatology visits (median 1.8 [0.6, 2.9]) per year) occurred more frequently than pulmonology visits (median 1.3 [0.5, 2.4]] per year) throughout the follow-up period. However, pulmonary visit frequency more closely correlated with PFT (r=0.51, p < 0.001) and chest CT (r=0.35, p < 0.001) testing frequency than rheumatology visits (PFT r=0.20, p < 0.001; chest CT r=0.09, p < 0.001). Baseline forced vital capacity negatively correlated with PFT (r=-0.13, p< 0.001) and CT (r=-0.04, p=0.01) testing rate.
Conclusion: RA-ILD monitoring is highly variable and appears to be sub-optimal (relative to idiopathic pulmonary fibrosis guidelines; Raghu et al. AJRCCM, 2022) in real-world settings. Sources of this variability could include the heterogeneity of the disease and prognosis, involvement of multiple medical specialties, a lack of evidence-based guidance for disease monitoring, and patient preferences, among others. These findings highlight the need for clinical practice guidelines on RA-ILD monitoring to inform rheumatologist and pulmonologist engagement in RA-ILD surveillance, particularly with the emergence of additional therapeutic options in RA-ILD.
To cite this abstract in AMA style:
England B, Johnson T, Yang Y, Roul P, Hershberger D, Sauer B, Cannon G, Baker J, Mikuls T. Real-World Disease Monitoring Patterns in Rheumatoid Arthritis-Associated Interstitial Lung Disease in the Veterans Affairs Health Care System [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/real-world-disease-monitoring-patterns-in-rheumatoid-arthritis-associated-interstitial-lung-disease-in-the-veterans-affairs-health-care-system/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/real-world-disease-monitoring-patterns-in-rheumatoid-arthritis-associated-interstitial-lung-disease-in-the-veterans-affairs-health-care-system/