Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Plain radiographs remain a cornerstone for diagnosis in rheumatology. Despite the importance of radiograph interpretation in rheumatology, there is little formalized instruction documented in the literature. The purpose of this curricular quality project was to develop and assess a virtual, instructional module for teaching internal medicine residents and medical students both general and rheumatology-specific radiology skills.
Methods: An interactive virtual module including musculoskeletal (MSK) radiographs was created and administered voluntarily to internal medicine residents and medical students at a single academic site. Participants were asked to complete a pre- and post-test to evaluate their knowledge and confidence in interpreting radiographs prior to and after participation in the module. Participants were also asked about their prior instructional experiences with MSK radiology. High-yield and commonly seen topics in the field of rheumatology including rheumatoid arthritis, psoriatic arthritis, gout, spondyloarthritis, and osteoarthritis were chosen based on relevance in terms of representation in the American College of Physicians Medical Knowledge Self-Assessment Program (MKSAP) and rheumatology attending decision. Fellows (n=4) and attendings (n=5) also completed the pre/post-test to evaluate whether this information is used in practice and learned over time.
Results: Forty-three trainees completed the pre-test. Thirty-three trainees completed the post-test. The average scores on the pre-test compared to the post-test improved from 4.5/10 to 6.5/10. Fellows and attendings scored 7.8/10 and 9.8/10, respectively. Student and resident scores on multiple topics, including identifying osteoarthritis, psoriatic arthritis, and rheumatoid arthritis on hand radiographs, improved after participation in the program (Table 1). Formal didactics reported in MSK radiology were low, particularly during residency (Figure 1). In the post-test survey, 52% of participants selected “somewhat agree” and 33% selected “strongly agree” when asked whether the module increased their ability to interpret MSK radiographs. Furthermore, confidence levels also increased (Table 2). One study limitation is that 10 participants did not complete the post-test.
Conclusion: Participating in this interactive module improved trainee scores and self-reported confidence in interpreting radiographs and diagnosing MSK conditions such as osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and spondyloarthritis. Though scores improved after participation in the module, many remained low. Next steps include reviewing content to improve identification of erosive OA, RA, and PsA changes and disseminating to other institutions to assess reproducibility. A structured curriculum surrounding the use of radiography in rheumatology is a useful tool for medical students and residents.
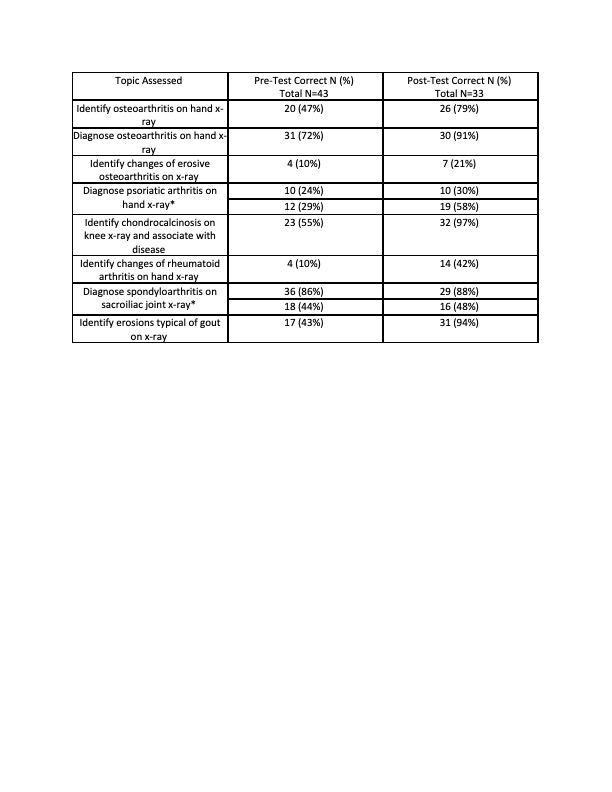 Pre and post test scores for topics assessed in interactive module.
Pre and post test scores for topics assessed in interactive module.
*Two separate questions were asked on diagnosis of psoriatic arthritis and spondyloarthritis
.jpg) Self-reported confidence level in diagnosing musculoskeletal conditions using radiographs
Self-reported confidence level in diagnosing musculoskeletal conditions using radiographs
.jpg) Musculoskeletal radiograph instruction methods reported by trainees
Musculoskeletal radiograph instruction methods reported by trainees
To cite this abstract in AMA style:
Konon E, Nichols L, Morcos M. RadRheum: Improving Resident and Medical Student Musculoskeletal Radiology Interpretation Skills Utilizing an Interactive Module [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/radrheum-improving-resident-and-medical-student-musculoskeletal-radiology-interpretation-skills-utilizing-an-interactive-module/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/radrheum-improving-resident-and-medical-student-musculoskeletal-radiology-interpretation-skills-utilizing-an-interactive-module/
