Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Racial disparities are prevalent in chronic illness, including pediatric rheumatic diseases. Prior work has investigated the impact of race on disease activity and damage in rheumatic diseases, such as lupus, but has not studied its impact on healthcare utilization patterns. As part of an institutional effort at the University of California, San Francisco (UCSF) to understand healthcare utilization of children with chronic illnesses who interact frequently with the healthcare system, we performed an analysis of rheumatology patients to describe healthcare utilization, including medication usage and communication with providers, by race. Our secondary aim was to investigate health disparities via the association between race and missed clinic visits, emergency department (ED) use, and inpatient hospitalizations.
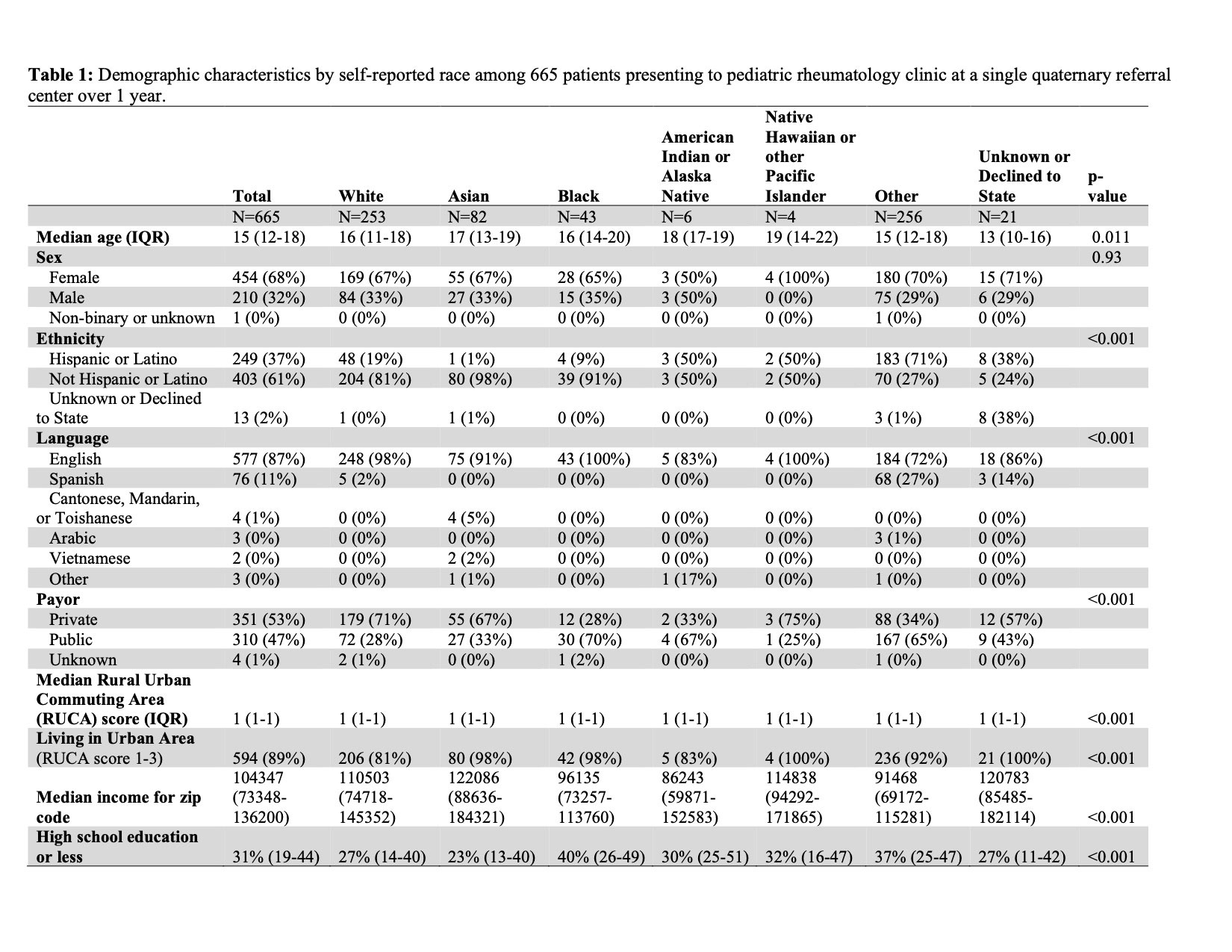
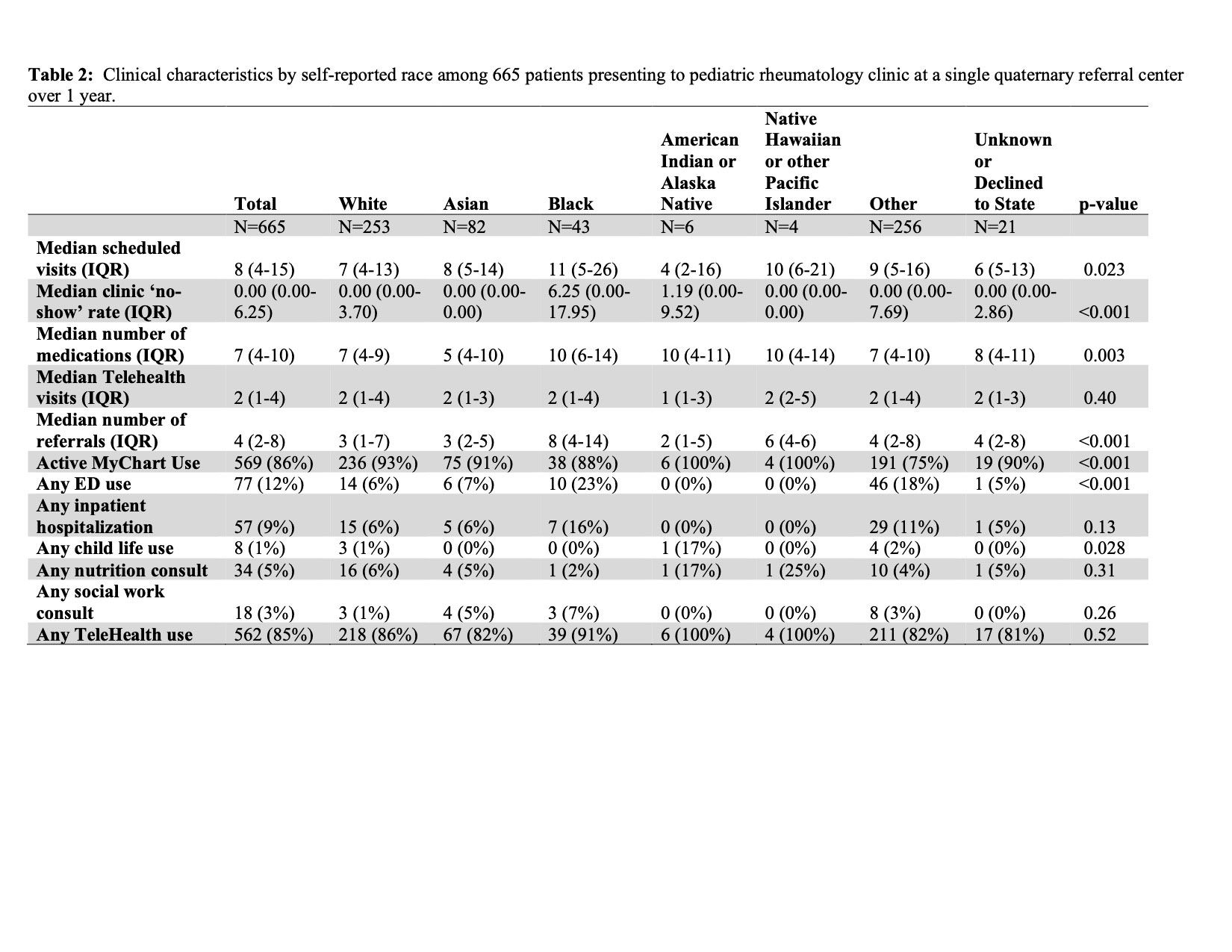
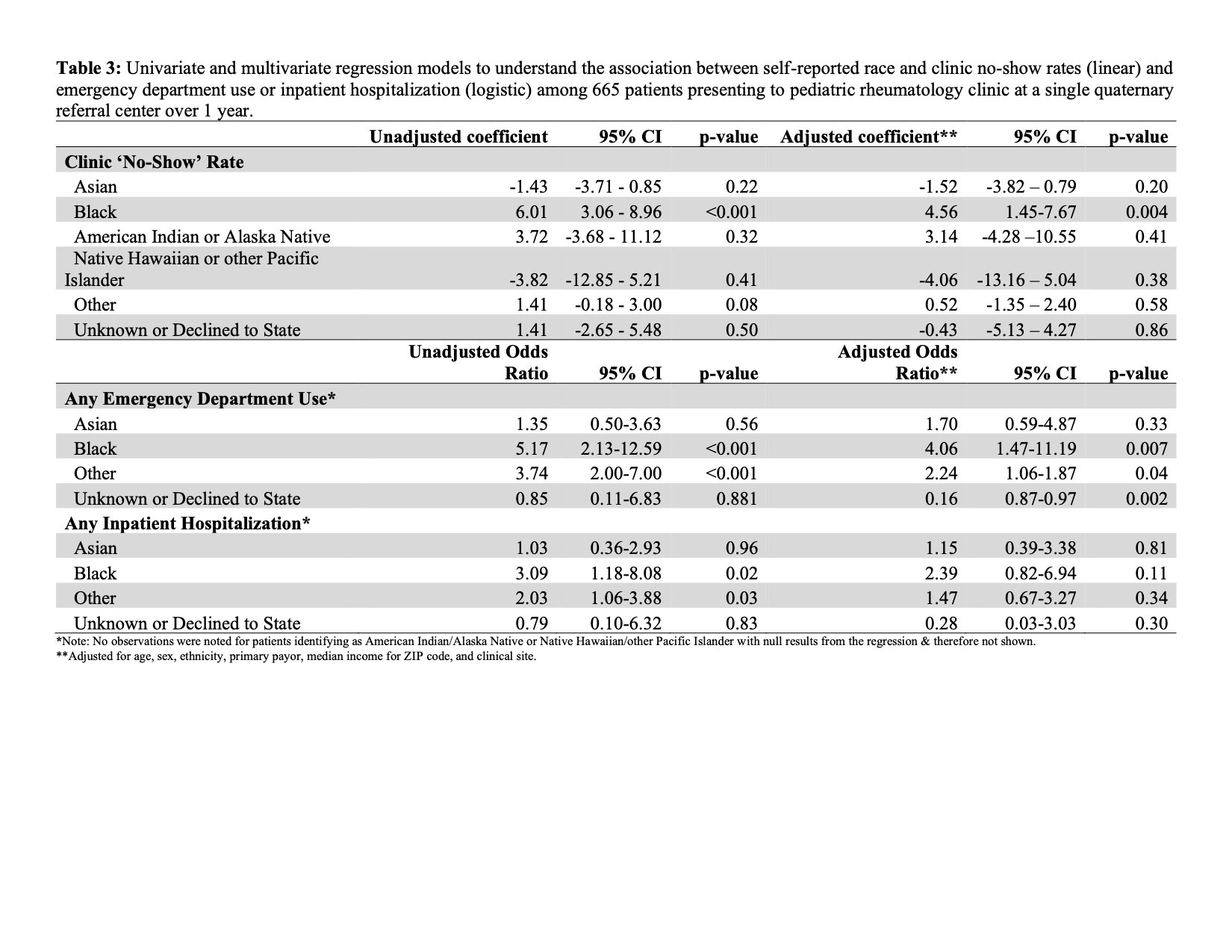
Methods: Patients defined as frequent presenters to pediatric rheumatology clinic at the UCSF (San Francisco and Oakland) were identified between 1/1-12/31/2021 by the presence of at least 6 healthcare encounters over a 3 year period with a primary subspecialty clinic in rheumatology. Demographic characteristics were collected, and socioeconomic measures were derived from 5-year estimates from the American Community Survey (ACS) 2020 survey data from the U.S. Census Bureau, including median income for zip code and guardian education. Urbanicity versus rurality was derived by geocoding 2010 Rural-Urban Commuting Area (RUCA) scores from the USDA. Descriptive statistics were performed using Kruskal Wallis and chi-squared tests, as appropriate, to describe the cohort by race. Univariate and multivariate (controlling for age, sex, ethnicity, median income for zip code, primary payor, and clinical site) regression models were created to investigate the association between race and missed clinic visits (linear) and any use of the emergency department or inpatient hospitalization (logistic).
Results: The cohort was predominantly ‘Other’ race (38%) or White (38%) (Table 1). White patients were mostly privately insured (71%) while Black patients (44%) and those identifying as ‘Other’ (51%) were predominantly publicly insured. 89% of the cohort lived in an urban area. Black patients had the highest number of scheduled visits (11) along with the highest ‘no-show’ clinic rates (6.25) (Table 2). Black and ‘Other’ race identifying patients also had the highest use of the emergency department (23% and 18%, respectively) and inpatient hospitalizations (16% and 11%, respectively). In multivariate modeling (Table 3), Black and ‘Other’ race were associated with missed clinic visits and ED utilization but not hospitalization, upon adjustment.
Conclusion: Black and multiracial patients have disproportionately high burden of clinic visits and subspecialty referrals along with ED use. Limitations include single center data that may limit generalizability of findings and inability to control for disease severity or diagnosis, which may confound findings. Future interventions may target lowering outpatient clinic visit burden and improving clinic show rates to understand if this may ameliorate the disproportionate usage of the ED compared to other racial groups.
**Adjusted for age, sex, ethnicity, primary payor, median income for ZIP code, and clinical site.
To cite this abstract in AMA style:
Soulsby W, von Scheven E. Racial Disparities Influence Healthcare Utilization in Pediatric Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-influence-healthcare-utilization-in-pediatric-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-influence-healthcare-utilization-in-pediatric-rheumatology-clinic/