Session Information
Date: Monday, November 13, 2023
Title: Abstracts: Pediatric Rheumatology – Clinical II: Connective Tissue Disease
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Social determinants of health (SDoH) contribute to disparate outcomes in both adult and pediatric systemic lupus erythematosus (pSLE), including length of hospitalization, mortality, and risk of severe sequelae, such as renal damage. Differential disease control may drive racial and ethnic disparities in disease damage and mortality. Therefore, we sought to determine how race associates with achievement of low lupus disease activity state (LLDAS), a clinically relevant disease activity target associated with higher health-related quality of life and less disease damage. We hypothesized that minoritized race would associate with lower rates of achieving LLDAS in the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Registry cohort of children with pSLE.
Methods: This was a cohort study of children with pSLE enrolled in the CARRA Registry between March 2017-December 2021 with baseline and at least one follow-up visit and a valid U.S. zip code. The primary exposure was self-identified race or ethnicity. SDoH of interest were insurance status and area deprivation index (ADI). The primary outcomes were 1) LLDAS and 2) occurrence of prednisone restarts or dose escalation between visits. Associations between race and/or ethnicity and the outcomes were examined using univariate and multivariable logistic regression models, adjusted for covariates (insurance status, ADI, age at enrollment, sex, major organ involvement, medication use, disease duration at enrollment, and secondary rheumatologic disease). Random effect was included in the LLDAS model to account for repeated measures.
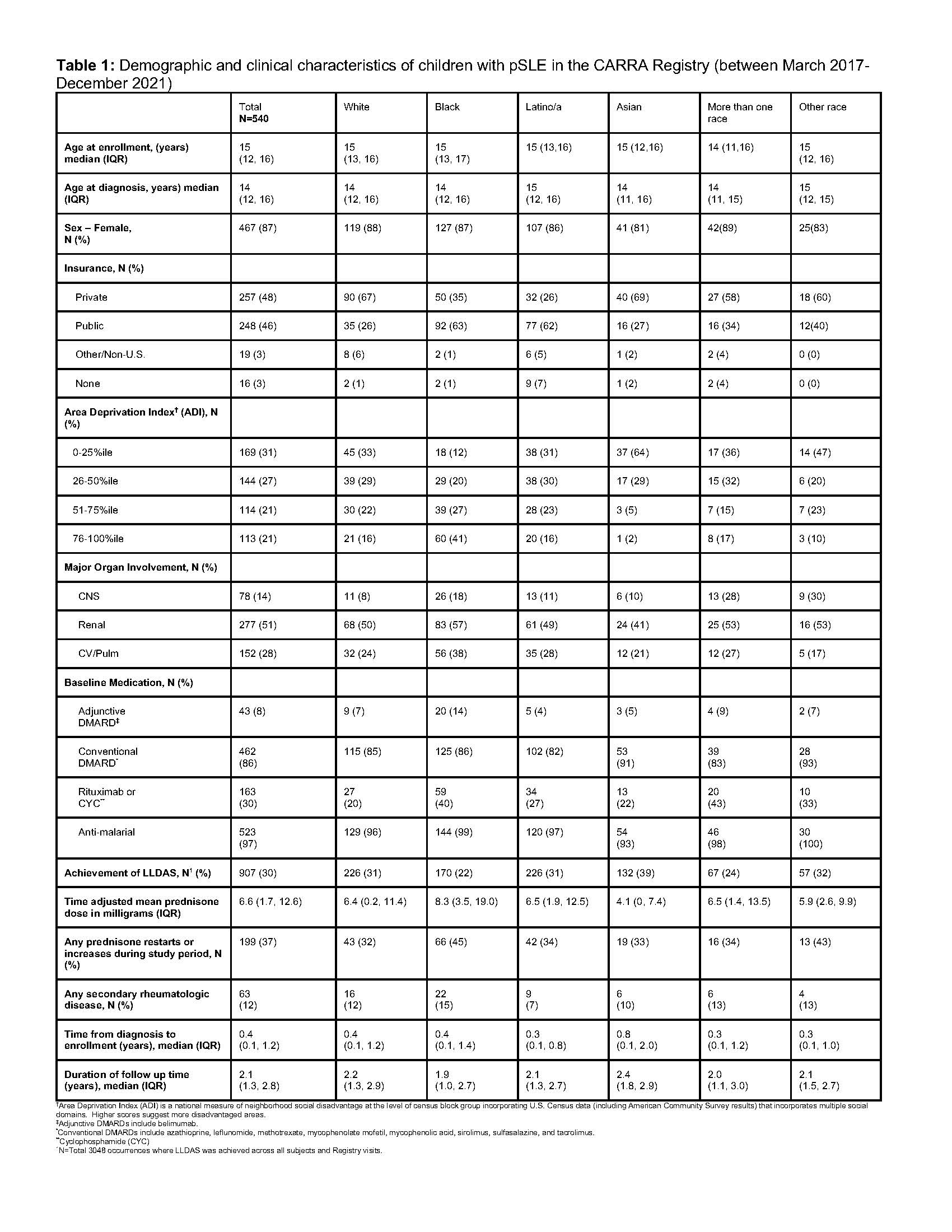
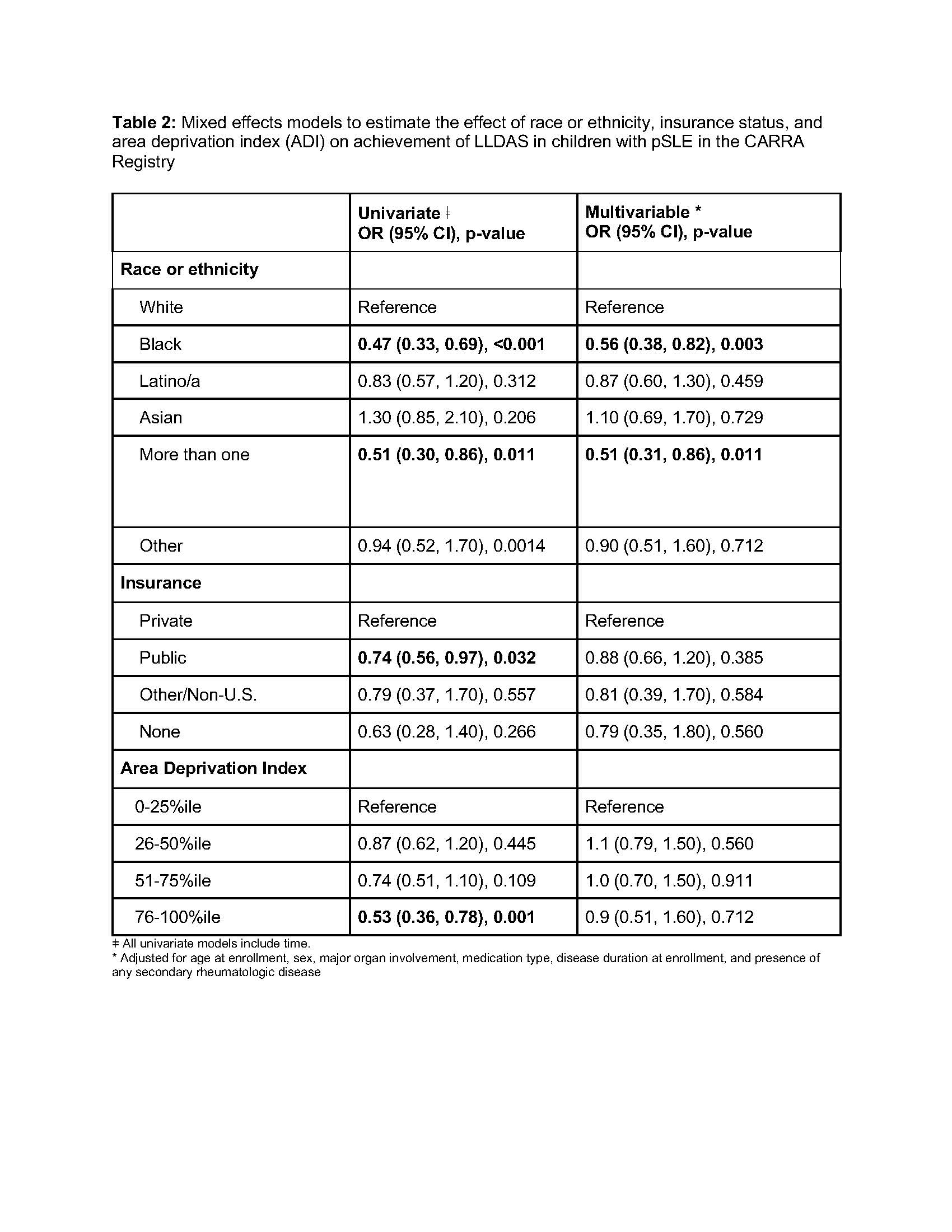
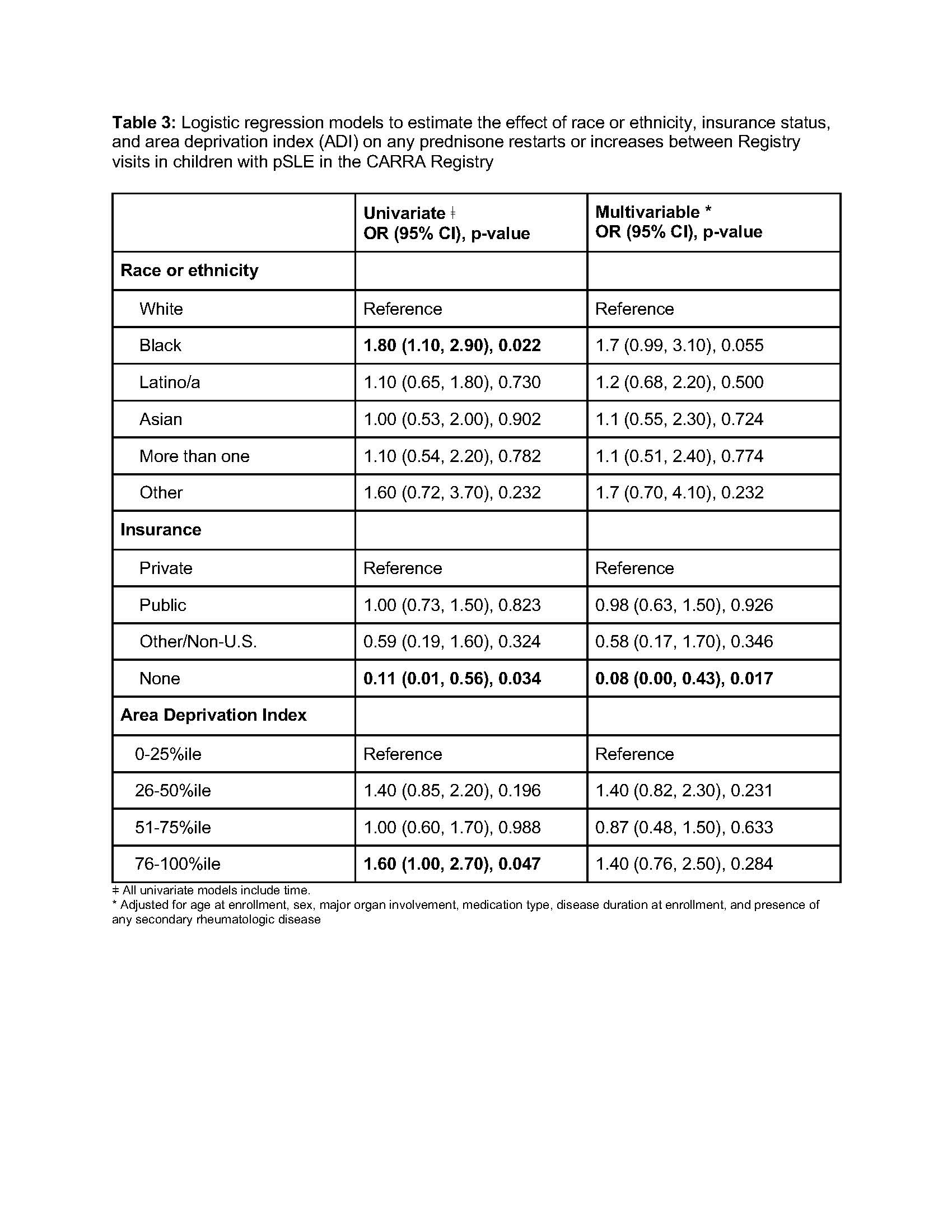
Results: A racially diverse cohort of 540 children with pSLE self-identified as 27% Black, 23% Latino/a, 25% White, 11% Asian, 5% Other, and 9% more than one race. 87% were female with a median age of 14.2 years at diagnosis (IQR 3.2-19.0). 48% were privately insured and 46% publicly insured. Black participants were more likely to be publicly insured, live in areas with higher social deprivation (ADI), and have renal disease (Table 1). In both unadjusted and adjusted analyses, Black race and more than one race were significantly associated with lower odds of achieving LLDAS (Table 2: adjusted OR 0.56, 95% CI: 0.38-0.82; OR 0.51, 95% CI: 0.31-0.86, respectively). In unadjusted analyses, Black race also associated with higher odds of prednisone dose increases or restarts. The adjusted estimate was similar, though not statistically significant at the 0.05 level (Table 3: OR: 1.7, 95% CI: 0.99-3.1, p=0.055).
Conclusion: Children with pSLE in the CARRA Registry identifying as Black or more than one race had significantly lower odds of achieving LLDAS. Black participants were more likely to be publicly insured and live in areas of higher social deprivation. Black race remained strongly associated with lower achievement of LLDAS despite adjustment for SDoH and disease characteristics. This suggests there are unmeasured factors driving the disparities, which may include other influences of structural racism, such as the experience of racial discrimination. Strategies to address these root causes will be important components of treat-to-target interventions designed to mitigate racial disparities in achievement of LLDAS.
To cite this abstract in AMA style:
Soulsby W, Olveda R, He J, Berbert L, Weller E, Barbour K, Greenlund K, Schanberg L, von scheven E, Hersh A, Son M, Chang J, Knight A. Racial Disparities Impact Achieving LLDAS and Glucocorticoid Use in Pediatric Lupus: A CARRA Registry Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-impact-achieving-lldas-and-glucocorticoid-use-in-pediatric-lupus-a-carra-registry-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-impact-achieving-lldas-and-glucocorticoid-use-in-pediatric-lupus-a-carra-registry-study/