Session Information
Date: Friday, November 6, 2020
Session Type: Plenary Session
Session Time: 11:30AM-1:00PM
Background/Purpose: In the US, cardiovascular disease (CVD) is the leading cause of disparities in life expectancy between black and white populations. We recently reported a 19-fold higher occurrence of CVD in blacks with SLE compared to non-blacks and noted disproportionately high stroke-related events around the time of SLE diagnosis. This study measured the risk and predictors of stroke and ischemic heart disease (IHD) in a predominantly black, population-based, incident cohort.
Methods: The Georgia Lupus Registry (GLR) is a population-based registry of SLE patients from Atlanta, Georgia. Incident patients in 2002-04 met ≥4 ACR SLE criteria or 3 criteria with a final diagnosis of SLE by their board-certified rheumatologist. Patients were matched to the Georgia Hospital Discharge Database and National Death Index from 2000-13. Stroke- and IHD-related hospitalizations and deaths were classified by the first three admission or cause of death codes. Stroke also included transient ischemic attack, and IHD included myocardial infarction and angina. Predictors of strokes and IHD were examined using Cox proportional hazards models.
Results: Among 336 incident SLE patients, 87% were female, 75% were black patient with a mean age at SLE diagnosis of 40 ± 17 years. There were 38 stroke-related and 25 IHD-related events or deaths, from the period 2 years before through 14 years after SLE diagnosis.
In the 11% with strokes, the mean age at first stroke was 48 years, with 78% occurring in females and 90% in blacks. The peak number of strokes occurred during the 2nd year after SLE diagnosis. We noted 8% had IHD, the mean age at first IHD was 52 years, with all occurring in females and 96% in blacks. The peak number of IHD occurred in the 14th year after SLE diagnosis.
Blacks had a 3-fold higher risk for stroke (HR 3.4, 95% CI 1.2-10, p 0.03) and a 24-fold higher risk for IHD (HR 24, 95% CI 3-206, p 0.004) (Table 1 & 2). Discoid rash at SLE diagnosis predicted a 5-fold (HR 4.6, 95% CI 1.7-13, p 0.003) and renal disorder predicted a 2-fold higher risk for stroke (HR 2.4, 95% CI 1.1-2.5, p 0.04) (Table 1). Neither impacted IHD (Table 2). Neurologic (HR 4.0, 95% CI 1.3-13, p 0.02) and immunologic disorder (HR 4.7, 95% CI 1.3-18, p 0.02) (Table 2) were strong predictors of IHD but not stroke.
Race stratified Cox proportional hazard models showed significantly accelerated stroke and IHD events in black compared to non-black patients (p ≤ 0.001) (Figure 1A & B).
Conclusion: We found a 3-fold higher risk of stroke and 24-fold higher risk of IHD in blacks with SLE. We found different SLE-specific predictors of stroke and IHD: discoid rash and renal disorder predicted stroke, and neurologic and immunologic disorder strongly predicted IHD. This study provides unique insights on significantly different SLE-disease related predictors, timing and racial disparities in stroke compared to IHD in SLE. Hence, we highlight the need to consider different preventive strategies for stroke and IHD in SLE.
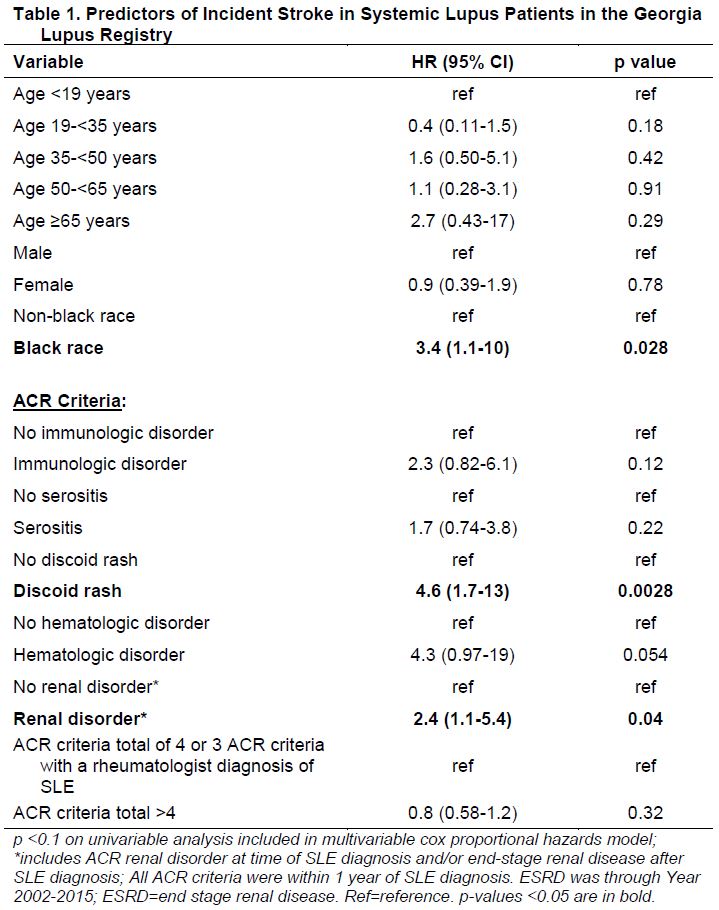 Table 1. Predictors of Incident Stroke in Systemic Lupus Patients in the Georgia Lupus Registry
Table 1. Predictors of Incident Stroke in Systemic Lupus Patients in the Georgia Lupus Registry
 Table 2. Predictors of Incident Ischemic Heart Disease (IHD) Occurrence
Table 2. Predictors of Incident Ischemic Heart Disease (IHD) Occurrence
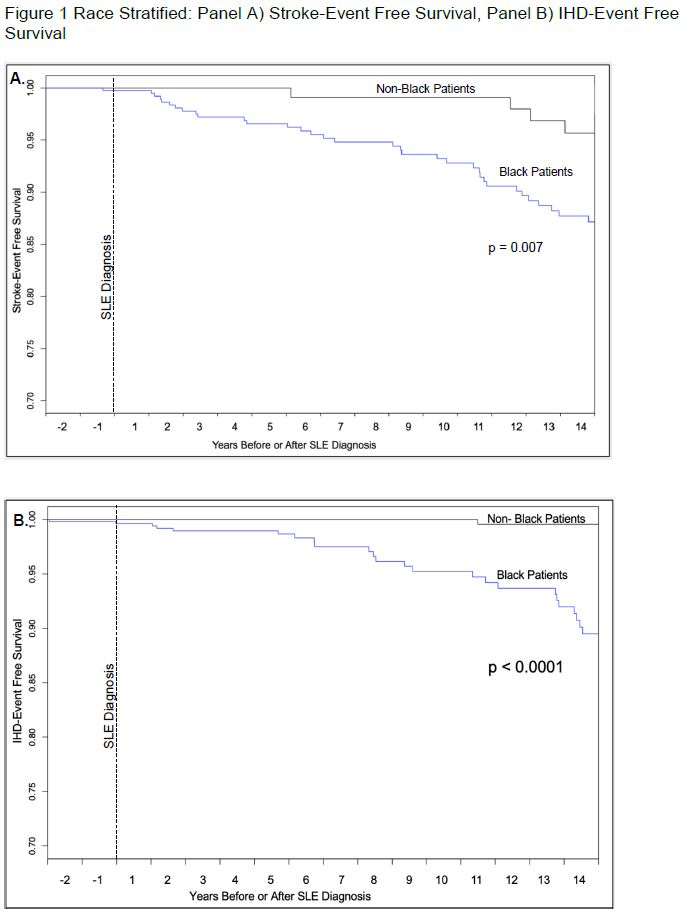 Figure 1 Race Stratified: Panel A) Stroke-Event Free Survival, Panel B) IHD-Event Free Survival
Figure 1 Race Stratified: Panel A) Stroke-Event Free Survival, Panel B) IHD-Event Free Survival
To cite this abstract in AMA style:
Garg S, Bartels C, Bao G, Drenkard C, Lim S. Racial Disparities and New SLE-Specific Predictors of Stroke and Ischemic Heart Disease in Patients with Lupus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/racial-disparities-and-new-sle-specific-predictors-of-stroke-and-ischemic-heart-disease-in-patients-with-lupus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-and-new-sle-specific-predictors-of-stroke-and-ischemic-heart-disease-in-patients-with-lupus/
