Session Information
Date: Saturday, November 6, 2021
Title: Abstracts: Healthcare Disparities in Rheumatology (0492–0495)
Session Type: Abstract Session
Session Time: 3:30PM-3:45PM
Background/Purpose: Glucocorticoids (GCs) are an integral part of systemic lupus erythematosus (SLE) treatment. Long-term use of GCs is associated with adverse effects. This study evaluated racial differences in GC use among individuals within the first year of SLE diagnosis.
Methods: Using Medicaid claims data (2000-2010) from 27 states, we identified individuals aged 18-65 years with incident SLE (>3 SLE ICD-9 codes separated by >30 days with no SLE codes in the 24 months before the first code [index date]). We required 1 year of continuous enrollment following the index date and >1 prescription for oral or intravenous GCs during that year. We calculated the prednisone-equivalent glucocorticoid dose (GD) for each 30-day period for 1 year following the index date. We constructed group-based trajectory models (GBTMs) to identify dynamic patterns of GC use. We examined baseline demographics, medications, comorbidities, and SLE-related clinical manifestations (SLE risk adjustment index, Ward, MM. J Rheum, 2001), in the 1 year prior to the index date. We used multinomial logistic regression to estimate the odds of being in the highest vs. lowest trajectory (OR, 95% CI). We estimated GBTMs stratified by race/ethnicity and updated covariates at 6 and 12 months to understand differences in GC patterns.
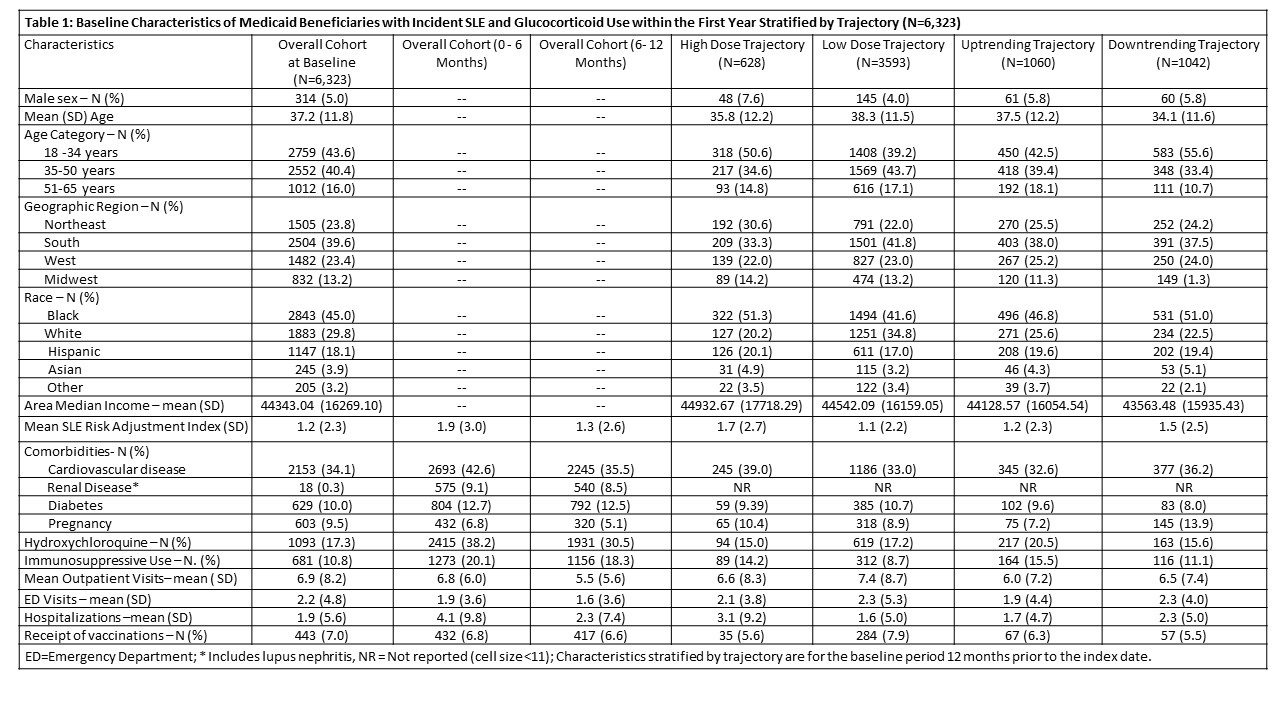
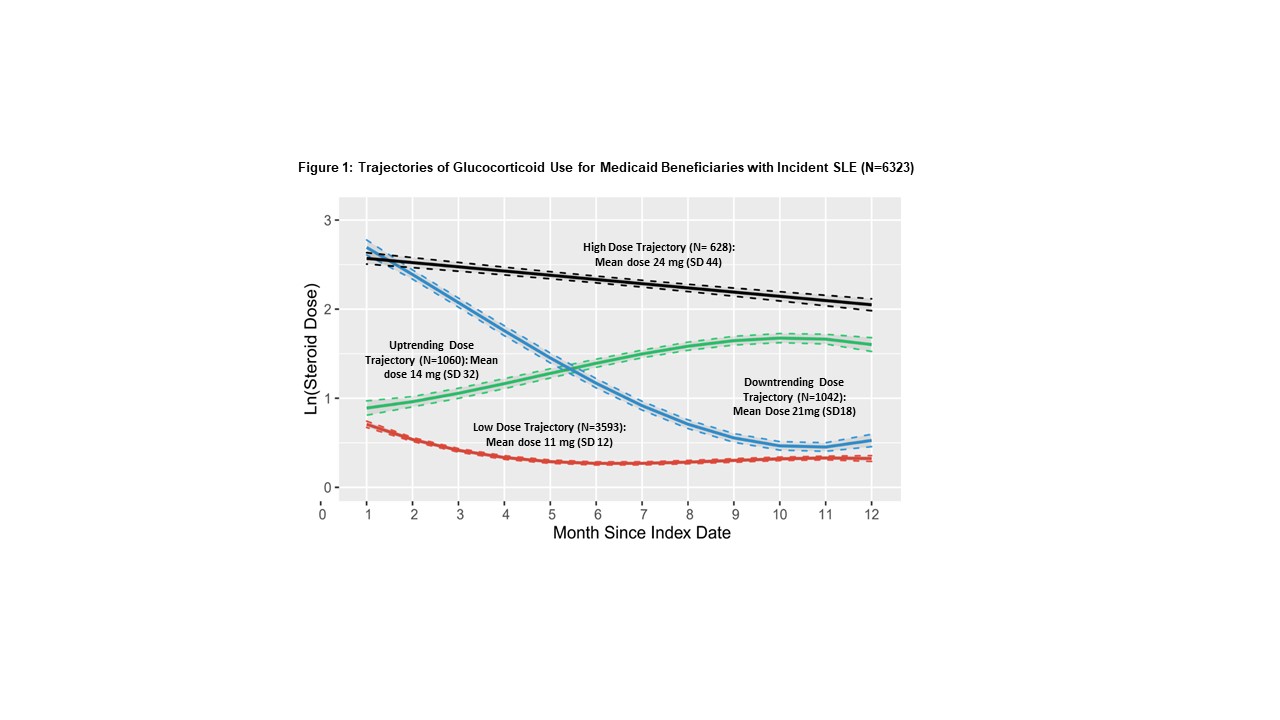
Results: Among 11,280 adults with incident SLE, 6,323 (53%) received >1 prescription for GC during the 1-year follow-up period. The mean (SD) age was 37 (12), 5% were male, 30% identified as White, 45% Black, 18% Hispanic, and 4% Asian (Table 1). The overall mean (SD) daily prednisone-equivalent GD was 18 mg (33) for Black patients, 17 mg (39) for Hispanic, 17 mg (17) for Asian, and 14 mg (14) for White. A four-group trajectory model for GC use and dose provided the best fit for the data (Fig 1). The highest trajectory of persistent moderate-to-high dose GC users included 628 individuals (10%); the mean (SD) GD was 24 mg (44). The lowest trajectory included 3593 individuals (57%); mean (SD) GD 11 mg (12). Multinomial models adjusted for demographics demonstrated greater odds of belonging to the highest vs. lowest steroid trajectory for Black (OR 2.23, 95% CI 1.77-2.80), Hispanic (OR 1.95, 95% CI 1.48-2.56), and Asian (OR 2.56, 95% CI 1.63-4.02) individuals vs. White; after adjusting for comorbidities, medications, healthcare use, and the SLE risk adjustment index, the ORs remained similar. In GBTMs stratified by race/ethnicity, Black, Hispanic and Asian individuals vs. White had more individuals in the highest GD and use trajectories. Comparing the highest GD utilizers by race/ethnicity during 0-6 month and 6-12 month intervals post-index date, there were no differences in immunosuppressive use. Black individuals had fewer outpatient visits and received fewer vaccinations than White individuals.
Conclusion: In this population of Medicaid beneficiaries with incident SLE, >50% received GC, and of those, 26% received at least moderate GC doses during the first year. While Black, Hispanic and Asian individuals had more SLE-related manifestations, this alone may not explain these differences. Access to high-quality outpatient care may be a modifiable factor that could address high dose GC use across racial/ethnic groups.
To cite this abstract in AMA style:
Chandler M, Santacroce L, Costenbader K, Desai R, Kim S, Feldman C. Racial Differences in Glucocorticoid Use Among Medicaid Beneficiaries with Incident Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-differences-in-glucocorticoid-use-among-medicaid-beneficiaries-with-incident-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-differences-in-glucocorticoid-use-among-medicaid-beneficiaries-with-incident-systemic-lupus-erythematosus/