Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Bone health in sarcoidosis is a complex topic, though data regarding racial differences in this population is lacking. Our study sought to identify racial differences in bone mineral density (BMD) and biochemical markers associated with bone metabolism in patients with sarcoidosis.
Methods: A retrospective study was performed on patients with a diagnosis code of sarcoidosis who received care at our tertiary sarcoidosis referral center and had undergone dual x-ray absorptiometry (DXA) scan between 2011 and 2019. Medical records were individually reviewed and data regarding demographics, sarcoidosis diagnosis and treatment, comorbidities, laboratory values and DXA results were abstracted. Data analysis used Chi square tests, Mann Whitney tests, and univariate and multivariate regression models in the R statistical environment (version 4.2).
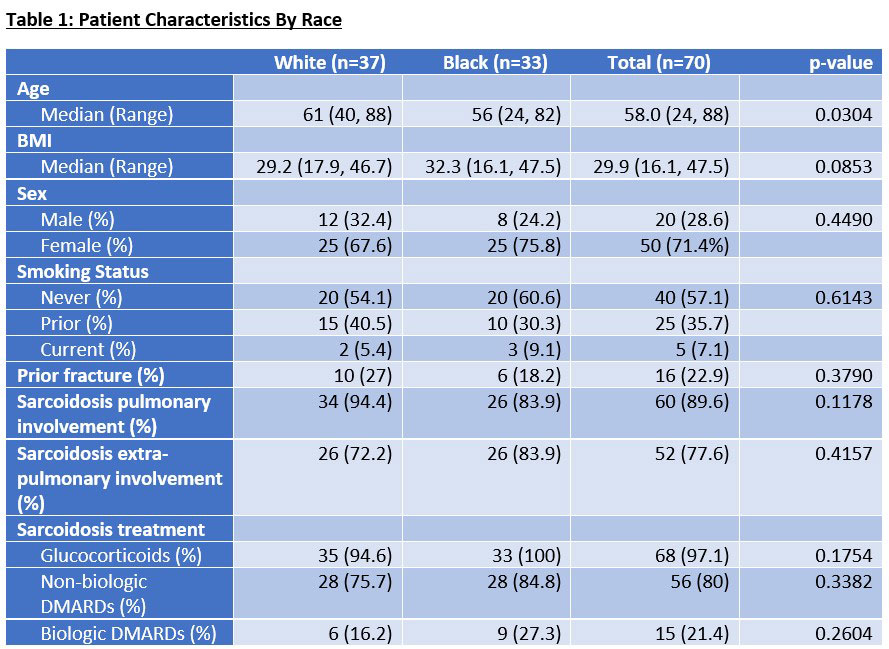
Results: We identified 70 patients who met inclusion criteria (Table 1). Thirty-seven (52.9%) were White and 33 (47.1%) were Black. Mean disease duration was 8 years with 60 (89.6%) having pulmonary involvement and 52 (77.6%) with other documented organ involvement. Sixty-eight (97.1%) of patients had received treatment with glucocorticoids, 56 (80%) with nonbiologic DMARDs, and 15 (21.4%) with biologic DMARDs. We were unable to calculate cumulative glucocorticoid dosing based on clinical documentation. Comorbidities did not differ significantly amongst racial groups.
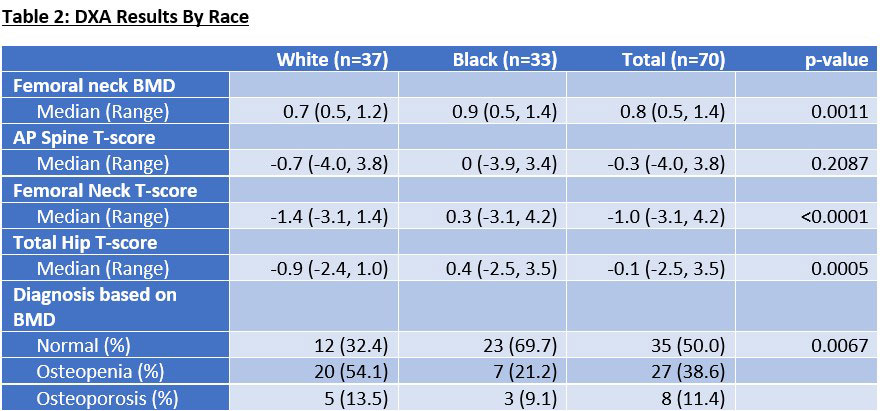
Eight (11.4%) patients were diagnosed with osteoporosis based on BMD and 27 (38.6%) with osteopenia. Older age and lower BMI were associated with reduced BMD (p=0.043 and 0.003, respectively) and this association was confirmed with a univariate logistic regression model.
Black subjects had significantly lower rates of osteopenia (21.2% vs 54.1%) or osteoporosis (9.1% vs 13.5%). A multivariate regression model, adjusted for age and BMI, showed that compared to White subjects, the odds ratio of a Black patient having low BMD was 0.308 (p=0.043, 95% CI 0.095-0.952).
As shown in Table 2, Black subjects had significantly higher T-scores than White subjects at the femoral neck (0.3 vs -1.4, p< 0.001) and total hip (0.4 vs -0.9, p=< 0.001), but not at the AP spine (0 vs -0.7, p=0.209). Black subjects were also more likely to have had a vertebral fracture assessment (VFA) performed, though only 1 out of 14 demonstrated a vertebral fracture.
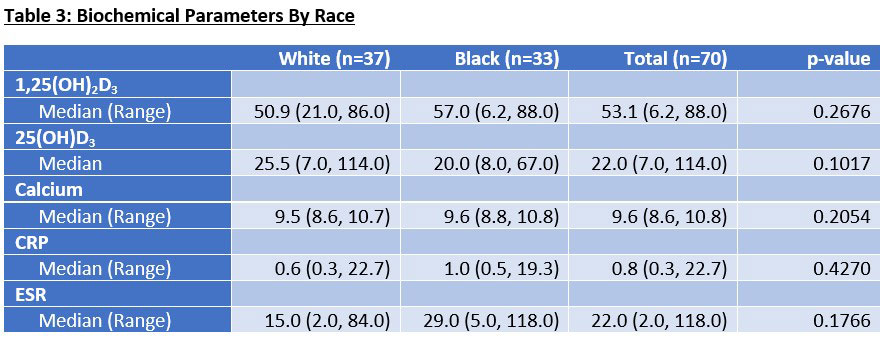
Analysis of biochemical parameters did not demonstrate any statistically significant differences amongst racial groups (Table 3).
Conclusion: Our study revealed that despite similar clinical and laboratory characteristics to White patients, Black patients with sarcoidosis had significantly greater femoral neck and total hip T-scores and less prevalence of osteoporosis or osteopenia. However, interestingly, vertebral T-scores were not significantly different between groups. This suggests that despite higher bone density at other sites, Black patients with sarcoidosis may have similar risk of vertebral fractures as their White counterparts.
To cite this abstract in AMA style:
Peninger E, Ascoli C, Lane R, Kukreja S, Baughman R, Sweiss N. Racial Differences in Bone Health of Sarcoidosis Patients: A Retrospective Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/racial-differences-in-bone-health-of-sarcoidosis-patients-a-retrospective-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-differences-in-bone-health-of-sarcoidosis-patients-a-retrospective-study/