Session Information
Date: Monday, November 8, 2021
Title: Epidemiology & Public Health Poster III: Other Rheumatic & Musculoskeletal Diseases (1022–1060)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Ensuring adequate representation of racial/ethnic minorities in research necessitates understanding the prevalence of rheumatic and musculoskeletal diseases in these populations. We sought to evaluate the relative prevalence of 8 rheumatic diseases across racial and ethnic groups within the National Patient-Centered Clinical Research Network (PCORnet), an integrated partnership of diverse health systems across the US that incorporate electronic health record data to answer clinical questions affecting patients’ lives.
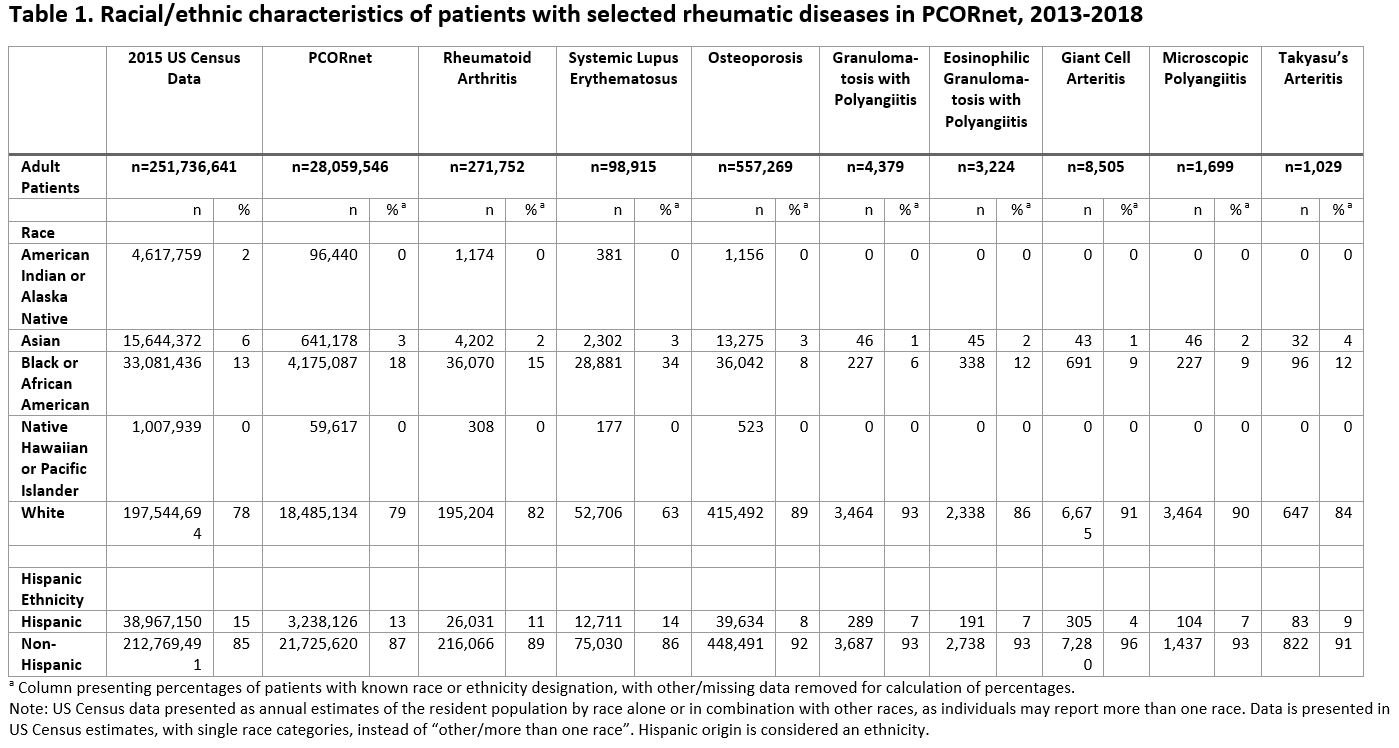
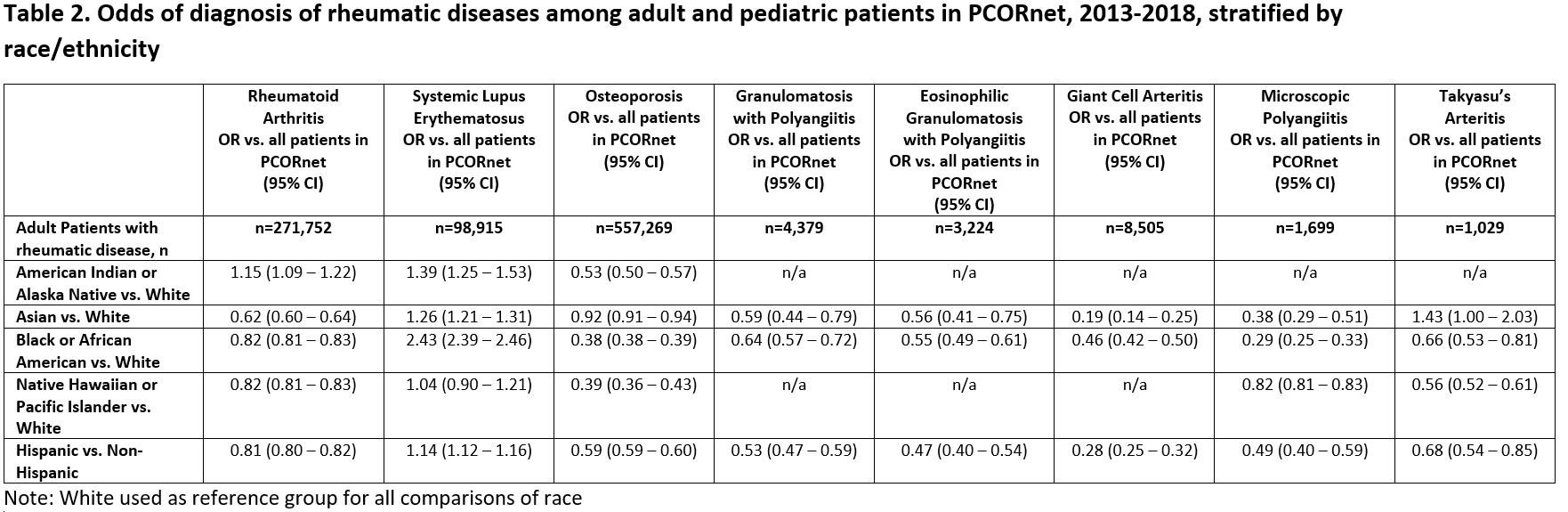
Methods: We queried electronic health records from 50 health systems of PCORnet from January 1, 2013 to December 31, 2018 and identified adult patients having ≥ 2 encounters separated by 90 days with diagnosis codes for rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), osteoporosis (OP), or several types of vasculitis (eosinophilic granulomatosis with polyangiitis (EGPA), granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), giant cell arteritis (GCA), and Takayasu’s arteritis (TAK)). We restricted to patients with race/ethnicity data and excluded those reporting more than one race or other. To assess representativeness of PCORnet data we compared racial/ethnic distributions in PCORnet to 2015 US census data. We then compared prevalence of rheumatic conditions across racial/ethnic groups to the PCORnet population and used univariable logistic regression to assess associations between race/ethnicity with different rheumatic diagnoses within PCORnet.
Results: A total of 28,059,546 adult PCORnet patients were included. Among the PCORnet patients with race/ethnicity data, 21% were non-white race and 13% Hispanic, similar to US Census data (Table 1). Compared to the wider PCORnet population, a higher percentage of adults with OP (89%) were white, while a higher percentage of patients with SLE (34%) were black/African-American (Table 1). African-American patients were more likely than white patients to have a diagnosis of SLE (OR 2.43, 95% CI 2.39-2.46, Table 2). American Indian/Alaska Native patients were more likely than white patients to have a diagnosis of RA (OR 1.15, 95% CI 1.09-1.22) and of SLE (OR 1.39, 95% CI 1.25-1.53), and Asian patients were more likely to have a diagnosis of Takayasu’s Arteritis than were white patients (OR 1.43, 95% CI 1.00-2.03).
Conclusion: Certain rheumatic diseases disproportionately affect people of color in the US population, and PCORnet, a data resource potentially useful for studying the epidemiology and outcomes of rheumatic and musculoskeletal diseases, mirrored these expected differences. An improved understanding of the demographics and epidemiology of rheumatic disease among patients of different races and ethnicities presents an opportunity to enroll patients into research studies in a more inclusive and representative manner, and will provide an improved framework for studies of genetic and/or environmental differences, and of clinical outcomes.
To cite this abstract in AMA style:
Nowell W, Barnes E, Parikh N, Venkatachalam S, Kappelman M, Curtis J, Merkel P, Shaw D, Young K, George M. Racial and Ethnic Distribution of Rheumatic Diseases in Health Systems of the National Patient-Centered Clinical Research Network [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-and-ethnic-distribution-of-rheumatic-diseases-in-health-systems-of-the-national-patient-centered-clinical-research-network/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-and-ethnic-distribution-of-rheumatic-diseases-in-health-systems-of-the-national-patient-centered-clinical-research-network/