Session Information
Date: Saturday, November 6, 2021
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Cardiovascular Pulmonary Disease (0268–0295)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) patients have 50% increased risk of heart failure (HF) vs non-RA patients with a distinct phenotype, preserved ejection fraction on transthoracic echocardiography (TTE) and attenuation of classic HF symptoms. Left ventricular (LV) remodeling (abnormal mass and wall thickness) is hypothesized to be an important precursor to clinical HF in the general population. Accordingly, LV structural abnormalities are prevalent in RA patients without clinical HF. Specifically, RA patients demonstrate higher mean LV mass index (LVMI) vs non-RA patients in cross-sectional TTE studies, with few correlates to RA associated inflammatory measures. However, prospective changes in LVMI and their significant clinical predictors remain poorly characterized in RA patients without clinical HF. Here we report on the evolution of LVMI in a prospective RA cohort without clinical cardiovascular disease (CVD), as well as its significant RA associated predictors, while adjusting for CV risk factors.
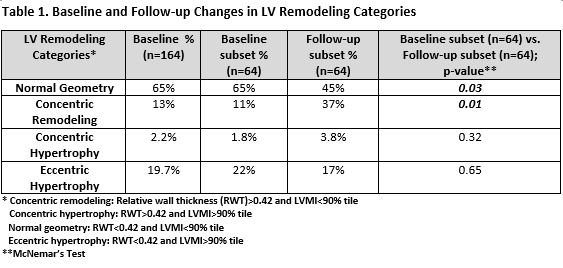
Methods: RA patients (n=164) without CVD underwent RA and CV clinical assessment and TTE at baseline. A subset (n=64) returned for follow-up TTE 3-6 years later. Real-time 3-dimensional (3D) echocardiography was utilized to calculate LV mass (indexed to height (m2.7)). LV remodeling categories [concentric remodeling (CRM), concentric hypertrophy (CH), and eccentric hypertrophy (EH)], utilizing the conventional cut-off for relative wall thickness (RWT) >0.42 and LVMI cut-off of >90% tile, were identified in the cohort (Table 1). Multivariable regression models (with LVMI as outcome) were utilized to adjust for biologically plausible confounders identified from univariable regressions.
Results: At baseline, up to 35% demonstrated abnormal LV geometry (CRM, CH, EH) and on follow-up this increased to 55% (Table 1). Specifically, the prevalence of CRM increased significantly from baseline to follow-up (p=0.01) (Table 1). The use of TNF inhibitors (TNFi) was associated (p=0.053) with higher baseline LVMI in multivariable models adjusted for RA and CV factors (no TNFi use vs TNFi use: 28.9 g/m2.7 vs 30.5 g/m2.7). On follow-up, mean LVMI increased 0.69 g/m2.7 per year but this was not statistically significant (p=0.82). The highest tertile of averaged CDAI was associated with the lowest increase in LVMI over time (from 0.86 g/m2.7 per year to 0.43 g/m2.7 per year) (Figure 1). Averaged CDAI also significantly predicted annualized rate of change in LVMI (p=0.046) (Table 2).
Conclusion: LV remodeling, particularly concentric remodeling, increased over time in RA patients without known CVD. At baseline, the use of TNF inhibitors was significantly associated with higher adjusted LVMI. On follow-up, higher averaged CDAI was associated with the lowest increase in LVMI. Further study is needed to clarify how lowering of RA disease activity through DMARD escalation impacts LVMI, and ultimately the development of clinical HF.
To cite this abstract in AMA style:
Park E, Ito K, Depender C, Giles J, Bathon J. RA Disease Activity Is an Independent Predictor of Left Ventricular Mass Changes in an RA Cohort Without Cardiovascular Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/ra-disease-activity-is-an-independent-predictor-of-left-ventricular-mass-changes-in-an-ra-cohort-without-cardiovascular-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ra-disease-activity-is-an-independent-predictor-of-left-ventricular-mass-changes-in-an-ra-cohort-without-cardiovascular-disease/